- Visibility 14 Views
- Downloads 3 Downloads
- DOI 10.18231/j.ijpi.2024.042
-
CrossMark
- Citation
Managing pyogenic granuloma: Insights from a case report
- Author Details:
-
Diksha Maurya *
-
Sanjay Gupta
-
Swapnil Agarwal
-
Shipra Singh
-
Tasneem Fatima
Introduction
Pyogenic granuloma (PG) is an inflammatory hyperplasia describing a large range of nodular growths of the oral mucosa.[1], [2] PG is a common non-neoplastic growth of the oral cavity, and the first case was described by Hullihen in 1844.[3] Even though various terms have been proposed earlier, Hartzell in 1904 gave the current term of PG or granuloma pyogenicum.[4] While this condition is frequently observed in the skin, it is infrequently encountered in the gastrointestinal tract, with the exception of the oral cavity, where it predominantly affects keratinized mucosa. Several factors, including persistent low-grade irritation, trauma, hormonal influences, and specific medications, have been identified as contributors to the onset of pyogenic granuloma (PG). In approximately 75% of instances, oral PGs manifest in the gingiva, with contributing factors such as inadequate oral hygiene, local irritants, and the presence of foreign materials in the gingival area.[5]
Numerous lesions that manifest in the oral cavity may resemble pyogenic granuloma (PG); however, a comprehensive patient history, thorough clinical assessment, and an appropriate treatment strategy are essential for accurate diagnosis. I have presented this case in which patient has given the history of Hepatits B with cleft palate along with swelling in lower front region of jaw in her IInd decade of life, so it’s necessary for the people to know about the circumstances associated with such conditions .This article will provide a case report of a significant pyogenic granuloma located in the gingiva of a 15-year-old patient, along with an extensive review of the relevant literature.
Case Report
A 15-year-old female presented to the Department of Periodontics with a complaint of swelling in the lower right anterior region of her jaw, which caused discomfort during meals. The patient indicated that she first observed the swelling two years prior; it was painless and fluctuant, showing no increase in size over that time. She ceased brushing the affected area because of bleeding and discomfort. Upon extraoral examination, no noticeable swelling was observed on the right side of the maxilla. The intraoral examination indicated a significant sessile lobulated gingival overgrowth on the facial surfaces of teeth 31, 32, and 33. This overgrowth was reddish-pink, exhibited irregular growth patterns, and measured approximately 20 mm by 45 mm. The surface was smooth, and no ulcerations were present. The surface exhibited a smooth texture, with no ulcerations observed. Oral hygiene was inadequate, and the associated teeth displayed no signs of mobility. A provisional diagnosis of pyogenic granuloma was established. The differential diagnoses considered included peripheral ossifying fibroma, peripheral giant cell granuloma, hemangioma, and fibroma. ([Figure 1])
The patient presented with a history of Hepatitis B and underwent repair of a cleft lip and palate at the age of one year. Consequently, the case was prepared for surgical intervention based on both clinical and pathological findings. To prevent the spread of infection, oral prophylaxis was conducted utilizing manual scalers. After one week, the patient was scheduled for the excision of the lesion under aseptic conditions. The excision, which included the mucoperiosteum, was performed under local anesthesia with a scalpel and #15 blade, followed by curettage and thorough scaling of the affected teeth. ([Figure 2]) The patient was then recalled for a follow-up appointment one week later. The excised tissue was forwarded to the Department of Oral Pathology for histological analysis. ([Figure 3], [Figure 4])
The histopathological examination indicated the presence of parakeratinized epithelium, which exhibited stretching in certain areas and demonstrated proliferation towards the base of the lesion. The underlying connective tissue stroma displayed dilated and engorged blood vessels, extravasated red blood cells, signs of angiogenesis, a limited number of inflammatory cells, and bundles of collagen fibers. The diagnosis of pyogenic granuloma was confirmed histologically. ([Figure 5])
The patient was scheduled for a follow-up appointment one week post-surgery, followed by another visit after one month for maintenance and to assess any potential recurrence. This case was monitored over a duration of six months, during which no recurrence has been observed to date. ([Figure 6])




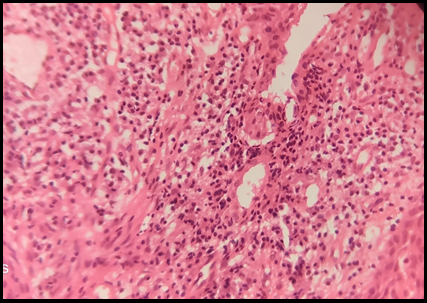

Granulation tissue with endothelial cell proliferation, dilated and engorged blood vessels, extravasated red blood cells, angiogenesis, a few inflammatory cells, and a bundle of collagen fibers were found by histopathologic analysis. ([Figure 5]) Clinical and histopathological characteristics were used to diagnose pyogenic granuloma.
Discussion
Pyogenic Granuloma is believed to originate from the periodontal ligament or the periosteum. The term "pyogenic granuloma" is considered misleading, as this condition does not result from granulomatous inflammation and does not contain pus. [6] In this case, pyogenic granuloma manifested in its most frequently observed location, specifically the anterior region of the mandible, in a female patient in her twenties. Intraorally, the gingiva is the primary site affected, followed by the lips, tongue, buccal mucosa, hard palate, mucobuccal fold, and frenum. The occurrence of Pyogenic Granuloma is consistent across both jaws, particularly on the labiobuccal surface of the marginal gingiva. [7] The estimated male to female ratio is approximately 1:1.15. [8] Elevated levels of estrogen and progesterone during puberty and pregnancy exacerbate pre-existing gingival inflammation by promoting the dilation and proliferation of blood vessels, as well as the release of vasoactive mediators from compromised mast cells. It is believed that trauma and female sex hormones may enhance the expression of angiogenic factors, such as basic fibroblast growth factor and vascular endothelial growth factor, contributing to the formation of pyogenic granuloma. [9] Pyogenic granuloma is believed to develop due to various factors, including hormonal imbalances, trauma from toothbrush use, the exfoliation of primary teeth, the eruption of permanent teeth, defective dental fillings in the area of the lesion, food impaction, and certain medications such as Cyclosporine. [10]
However, in the present case, trauma from tooth brush has been implicated in etiopathogenesis of oral pyogenic granuloma. As aetiology in our case includes calculus and trauma, Kerr and Ainamo studies discovered that recurrent trauma causes release of various endogenous and angiogenic which contributes and increases vascularity of the lesion. [11] The differential diagnosis for reactive lesions of the gingiva must encompass pyogenic granuloma, fibrous hyperplasia (also known as fibrous epulis), peripheral giant cell granuloma, and peripheral odontogenic fibroma. The literature presents several treatment options for pyogenic granuloma, including scalpel excision, laser therapy, cryotherapy, and electrocauterization. While these treatment modalities have demonstrated effectiveness, each comes with its own set of advantages and disadvantages. The various treatment options available indicate that both Laser and Electrosurgery have been associated with damage to surrounding tissues and prolonged wound healing. In contrast, the bloodless surgical field has been noted to enhance patient comfort, reduce pain, and facilitate healing without the formation of scars. [12] In this instance, the scalpel method was selected over the a forementioned techniques imitigate the risk of infection, particularly given the patient's Hepatitis B status.
Conclusion
This article aims to present a comprehensive report on a significant pyogenic granuloma (PG) located in the mandibular gingiva. It includes an in-depth examination of the aetiologies, clinical characteristics, histological findings, differential diagnoses, treatment options, and recurrence rates associated with this condition. Although PG is a frequently encountered lesion, possessing a thorough understanding of its nature is essential for distinguishing it from other similar clinical manifestations, thereby ensuring that appropriate treatment strategies are employed to achieve optimal outcomes.
Source of Funding
None.
Conflict of Interest
None.
References
- MS Greenberg, M Glick. . Burket’s Oral Medicine. Diagnosis and Treatment 2003. [Google Scholar]
- LR Eversole. . Clinical Outline of Oral Pathology. Diagnosis and Treatment 2002. [Google Scholar]
- SP Hullihen. Case of Aneurism by Anastomosis of the Superior Maxillare. Am J Dent Sci 1844. [Google Scholar]
- MB Hartzell. Granuloma pyogenicum. J Cutan Dis Syph 1904. [Google Scholar]
- SR Gomes, QJ Shakir, PV Thaker, JK Tavadia. Pyogenic granuloma of the gingiva: A misnomer? - A case report and review of literature. J Indian Soc Periodontol 2013. [Google Scholar]
- E S Goncales, J H Damante, C M Fischer Rubira, L A Taveira. Pyogenic granuloma on the upper lip: An unusual location. J Appl Oral Sci 2010. [Google Scholar]
- R Kamal, P Dahiya, A Puri. Oral pyogenic granuloma: Various concepts of etiopathogenesis. J Oral Maxillofac Pathol 2012. [Google Scholar]
- AS Al-Noaman. Pyogenic granuloma: Clinicopathological and treatment scenario. J Indian Soc Periodontol 2020. [Google Scholar]
- AO Ojanotkoharri, MP Harri, HM Hurttia, LA Sewon. Altered tissue metabolism of progesterone in pregnancy gingivitis and granuloma. J Clin Periodontol 1991. [Google Scholar]
- C Rossa, A Cartagena, A Torre. Oral pyogenic granuloma diagnosis and treatment: A series of cases. Rev Odontol Mex 2017. [Google Scholar]
- J Ainamo. The effect of habitual toothcleansing on the occurrence of periodontal disease and dental caries. Suom Hammaslaak Toim 1971. [Google Scholar]
- K Debnath, A Chatterjee. Management of recurrent pyogenic granuloma with platelet-rich fibrin membrane. J Indian Soc Periodontol 2018. [Google Scholar]
