Introduction
Gingival overgrowth (GO) can be described as an enlargement of the gingival tissues. GO may manifest as a localised or a generalised condition which is caused by several other underlying factors.1 Therefore, it is always considered pathological which causes esthetic, masticatory, functional, and psychological disturbances for the patients.2 Hence, it is vital to treat such conditions GO can be classified as ‘plaque-induced’ and non-plaque-induced; however, often a more definite primary etiology can be found.3 The foremost step in treating GO is maintaining the patient’s oral hygiene which includes mechanical debridement of plaque and calculus, motivating the patient and also removal of any other etiological factor associated with GO. However, non-surgical periodontal treatment is not always effective when the condition is extensive and associated with some other underlying cause. Therefore, a surgical intervention (gingivectomy) becomes mandatory in order to return the gingiva to its anatomical and physiological position. 4
Gingivectomy is a procedure in which the unsupported gingival tissue is excised, thus creating a fresh gingival margin that is apical to the former margin.5, 6 Gingivectomy can be carried out with a variety of techniques, including scalpels, electrosurgery, chemosurgery, and lasers. The conventional surgical technique using scalpel is easy to use, accurate and causes minimal damage to the tissue.7 However, they do not deliver a good haemostasis, which becomes essential while incising a highly perfused tissue like gingiva.6 Laser stands for ‘Light Amplification by Stimulated Emission of Radiation’. The first laser device, Ruby laser was invented by Maiman in 1960.8 Diode lasers are highly absorbable by melanin and haemoglobin allows soft tissue manipulations providing sound results in periodontal surgery.9 With laser the major advantages are the production of local hemostasis, thereby creating a virtually blood less surgical field and bacterial elimination. 10, 11
Despite the potential advantages, there are only few studies comparing traditional method of gingivectomy versus diode laser-assisted gingivectomy, therefore, this trial was conducted to evaluate and compare the effects of diode laser on intra and post-operative parameters over conventional scalpel gingivectomy.
Materials and Methods
Study design
The patients visiting the Department of Periodontology, H.P. Government Dental College and Hospital, Shimla were selected for the present prospective randomized controlled trial (RCT). The study protocol was approved by the institutional ethical committee [No:(HFW(GDC)B(12)50/2015 3349] and was conducted in accordance with Helsinki’s guidelines for RCT. The CONSORT statement was used for the reporting of the study. 12
Study sample
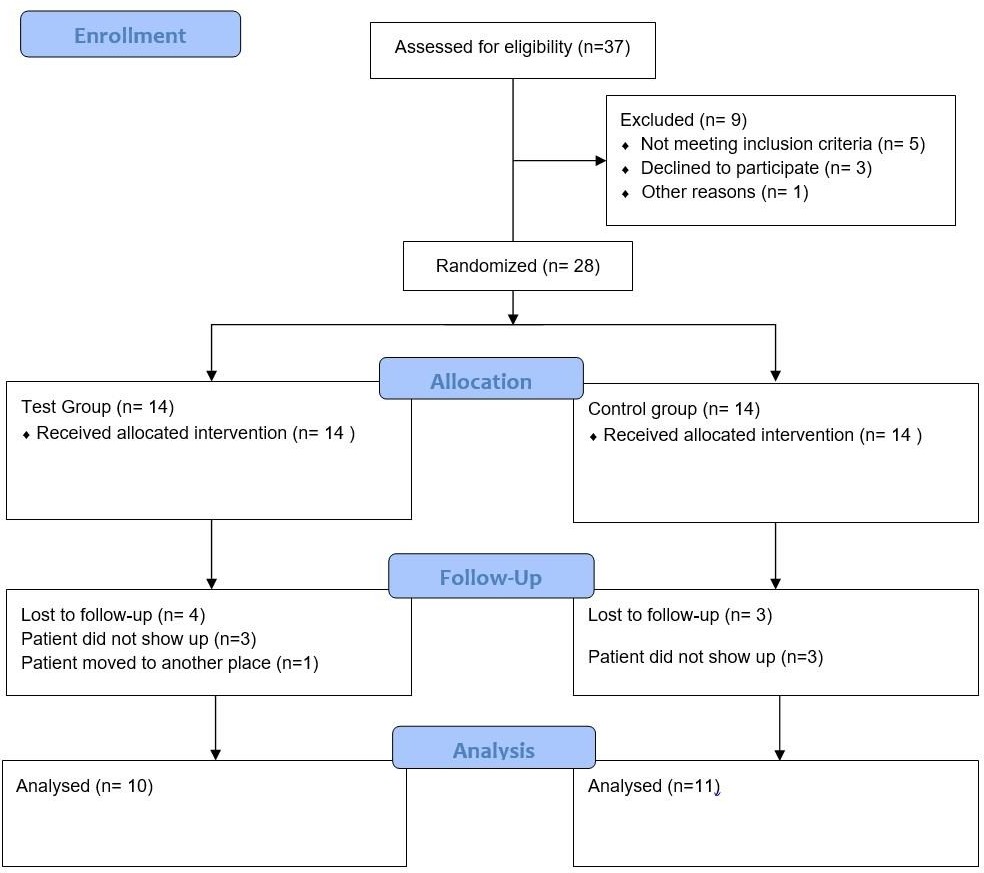
The patient selection, surgical procedure and follow-up were performed from February 2021 to September 2022. A total of 21 patients (13 male and 8 female), 10 in the test group and 11 in the control group, with a mean age of 33.8 years and with localized or generalized GO were enrolled in the study. All eligible patients signed an informed consent form and were thoroughly explained about the treatment, potential risks and benefits of their participation in the study. A total of 20 patients were required. However, considering that some patients could be lost to follow-up, 28 patients were enrolled in this study (Figure 1). A double-blinded, RCT was designed. The subjects were randomly divided into two groups, using coin and toss method.
Test Group – (Gingivectomy performed with diode LASER)
Control Group- (Gingivectomy performed with scalpel)
Inclusion criteria
Subjects with localised or generalised suprabony pocket ≥4mm in depth.
Inflammatory gingival enlargement
Subjects between 18-60 years of age.
Patients who consented to participate in the study.
No history of previous surgical treatment in the selected area.
Systemically unhealthy patients, smokers, pregnant and lactating females were excluded from the study.
Initial therapy and clinical measurements
Presurgically, a specialist in periodontist (MSW), who was blinded to the experimental groups, performed supragingival and subgingival SRP. All the measurements were performed by a single trained examiner using UNC-15 periodontal probe prior to the surgery and also 1 and 3 months after the surgery. The following clinical parameters were assessed. Parameters in this study were divided into two groups, intraoperative and post-operative parameters.
Intra-operative parameters
Hemostasis or bleeding was scored as: 1: None; 2: Self-limiting; 3: Requiring light pressure; 4: Requiring coagulation and 5: Requiring ligation or Hemoclips Duration of surgical procedure was measured in minutes.
Post-operative parameters
Probing Pocket Depth (PPD): the distance between the gingival margin and the tip of the periodontal probe inserted into the sulcus with a force of 0.25 N.
Wound healing index: which was assessed clinically at the 10th day, 1 month and 3 months postoperatively using the Landry index.13 ranging from score 1 (Very poor) to 5 (Excellent).
Postoperative pain which was evaluated by 10-point Visual Analog Scale (VAS) at 24hr and 72hrs interval after surgery ranging from 0 (no pain) to 10 unbearable pain).
Based on the average VAS score for each group, patient comfort for each surgical procedure was evaluated. Score was given as follows:
0-2- Fully comfortable
3-5- Slightly uncomfortable
6-10- Highly uncomfortable
Surgical preparation
All the surgical procedures were performed by one operator (NC). Extraoral preparation with 5% Povidone Iodine solution was done, also the patients were asked to rinse with 10 ml of 0.2% chlorhexidine digluconate solution for 1 minute.
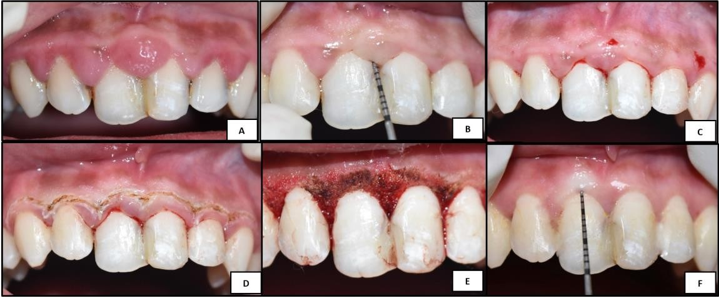
Test group (LASER) (Figure 2)
After the area was adequately anaesthetized with topical lidocaine or injectable 2% lidocaine with 1:80 000 adrenaline, the clinician and the patient put on safety precautions such as safety glasses for the laser-assisted gingivectomy. A diode LASER (MEDENCY) with pre-set wavelength was used in a contact type mode. The LASER unit was used with a setting of 8.5W in continuous mode along the previously demarcated area in a paint brush-like strokes progressing slowly for removing the gingival tissue and expose an adequate amount of tooth structure. Throughout the procedure, the tip was repeatedly inspected for ablated tissue debris and cleaned using clean moist gauze. Physiological gingival contour was achieved by changing the angulation of the tip as required during the procedure.
Control group (Scalpel) (Figure 3)
Patients were anaesthetized with 2% lidocaine and 1:80 000 adrenalin. When sufficient anesthesia was achieved, transgingival probing was performed in order to mark a reference point serving as the visual finishing point indicating the CEJ. After determining the total amount of gingival tissue to be removed, an external bevel incision was made using a scalpel blade (No. 15) and the gingival tissue was excised with gingivectomy knife. Following excision of the enlarged tissue, gingivoplasty was performed to remove any left out tissue tags to attain a smooth surface.
Periodontal dressing (Coe-Pack was given in both the groups for 10 days.
Postsurgical care
Postoperative instructions were given to the patient and analgesic (tablet Aceclofenac 100 mg) was prescribed twice daily for 3 days. Patients were instructed not to brush the operated site for atleast 10 days and advised to rinse the oral cavity with chlorhexidine 0.12% mouthwash. After 10 days the periodontal dressing was removed and the surgical site was assessed. Patients were recalled 1 month and 3 months after surgery and clinical recordings were taken.
Statistical analysis
Clinical records were taken at the pre-defined intervals (pre-operative, immediately after surgery, 10 days post-operative and at 1 and 3 months post-operative). For intragroup variation ‘Wilcoxon Signed-Rank Test’ was performed and for intergroup comparison ‘Unpaired t test’ and ‘Mann-Whitney U Test’ was performed. All values of P < 0.05 were considered as significant and ≤0.001 were considered as highly significant difference.
Results
All the treated sites healed without any complications and the surgical procedure was well tolerated by all the patients. 4 patients in the test group and 3 in the control group did not report for the follow up. Hence, a total of 10 patients in the test group and 11 in the control group were included for the data analysis.
Intra-operative parameters
Better hemostasis was observed in the test group than the control group with a statistically significant difference (p=0.001) (Table 1). In the test group the mean time taken for the surgical procedure 26.8±5.84 minutes, while in the control group the mean time was 27±5.31 and the difference was not statistically significant (p=0.44) (Table 2).
Post-operative parameters
The healing in the test group was better than in the control group and was statistical significant when recorded at 10th day (p=0.001), 1 month (p=0.02) post, but no statistical difference was observed at 3 month post-operatively (p=0.25) (Table 3). The PPD in the decreased from 5.5 ±1.10 mm at baseline to 0.4 ±0.32 mm at 3 months (p = 0.002), while it decreased from 5±0.64 mm to 0.82 ±0.4 (p=0.001) in the control group and was statistically significant. No significant differences between both the groups were found in the PPD (Table 4). The intergroup comparison showed higher VAS score in the control group when compared to the test group and was statistically significant at 24hrs (p=0.0002) and at 72 hrs (p=0.002) (Table 5). Based on the mean VAS score recorded at 24hrs and 72hrs post operatively, patient comfort level was interpreted. The mean VAS score in the test group at 24hrs and 72hrs interval was 1.3 and 0.6 respectively, while for the control group it was 3.5 and 2.1 respectively. Hence, it was interpreted that patients were fully comfortable in the test group till 72 hrs post operatively, but in the control group patients were slightly uncomfortable after the procedure.
Table 1
Showing intergroup comparison of bleeding scores for Test and Control group (intra-operative)
|
|
Test group |
Control group |
p value |
||
|
|
n=10 |
% |
n=11 |
% |
|
|
1-None |
8 |
80 |
0 |
0 |
0.001** |
|
2-Self-limiting |
2 |
20 |
2 |
18.8 |
|
|
3-Require pressure |
0 |
0 |
9 |
81.2 |
|
|
4-Require coagulation |
0 |
0 |
0 |
0 |
|
|
5-Require ligation |
0 |
0 |
0 |
0 |
|
Table 2
Table showing intergroup comparison of duration of the surgery for test and control group
|
|
Test group (n=10) (Mins) |
Control group (n=11) (Mins) |
p value |
|
Duration of the surgery |
26.8±5.84 |
27±5.31 |
0.44# |
Table 3
Table showing Inter group comparison of Healing in test and control group at10th day, 1 month and 3 month
Table 4
Table showing inter group comparison of PPD at baseline and 3 months
Table 5
Table showing intergroup comparison of the VAS score at 24hrs and 72hrs post-operative
Discussion
Different treatment modalities, which have been reported for treating GO, but the use of scalpel for gingivectomy is a time tested technique and remains the gold standard as it is most economical compared with other techniques, which require more advanced armamentarium. 7, 14 However, with scalpels it is difficult to achieve a good haemostasis. An alternative to which is the laser gingivectomy, which offers potential advantages of sterilization of the surgical field and reduced haemorrhage during excision. 15 Moritz et al16 in an in vitro and in vivo study showed a bactericidal effect of diode laser because of the rise in temperature. Among all the different types of lasers, diode laser has gained increasing importance and interest as it has energy and wavelength characteristics that specifically target the soft tissues, also is portable and can be easily managed. 17
In addition, laser surgery greatly reduce the rate of recurrence of GO,14 which may be attributed to decrease collagen production by gingival fibroblasts.18 In addition, laser surgery greatly reduce the rate of recurrence of GO, 14 which may be attributed to decrease collagen production by gingival fibroblasts.19 When comparing the intra-operative parameters no bleeding was observed in majority of the patients in the control group. The finding agrees with the other studies,15, 20, 21, 22 which concluded that virtually bloodless field is observed while using lasers. This could be attributed to the fact that the laser causes coagulation and vaporization at the surgical site due to rise in temperature, in turn seals the blood vessels. 11, 23 During the wound evaluation, none of the surgical sites showed excessive granulation tissue or bone denudation. Wound healing after Laser gingivectomy is debated. Some investigators reported delay healing when compared to scalpel gingviectomy,11, 24, 25 while some research shows that healing of laser wound is either similar or accelerated than scalpel wound. 15, 26, 27, 28 However, the wound healing after laser gingivectomy is greatly affected by the laser parameters such as power, frequency, pulse duration and exposure time. 8
It was quite evident that the healing post-surgery in the test group was better than in the control group during the initial phase of healing in this present study. This observation can be correlated to the fact that laser treatment causes little or no damage to the underlying connective tissue matrix and in addition the basement membrane resists laser irradiation. 15 The laser-induced wounds heal through reparative synthesis of matrix proteins. The slow removal and replacement of the residual matrix accounts for the lack of scarring and contraction observed in laser-treated areas. 6 The present study results are in alignment with other studies 6, 16, 29 which concluded laser irradiation could have beneficial effect on the wound healing.
There was a noteworthy connotation between the type of treatment and postoperative pain. The patients in test group had almost no postsurgical pain recorded at 24hrs and 72hrs post operatively when compared to control group. The average VAS score at 24hrs and 72hrs was higher in the control group than in the test group. This could be explained by the fact that, the heat generated by laser inhibits the pain receptors and the protein coagulum that is formed on the surgical site by laser acts as a biologic dressing which seals the sensory nerve endings.6 The results obtained in the study are similar to study done by Pick & Colvard (1993) 26 and Hadeel Mazin Akram et al.(2017).6 Based on the mean VAS score, patients in the test group were rate ‘fully comfortable’ during and after the procedure, but patients in the control group were rate ‘slightly uncomfortable’ because of slightly higher VAS score. Therefore it was concluded that lasers were better accepted by the patients. Hadeel Mazin Akram et al. in 2017,6 also concluded that pain and discomfort level in patients treated with scalpel was higher than the patients treated with laser gingivectomy. Although the results showed statistically significant difference between the two groups, the small study group necessitates the future studies with a large sample size and long term follow up.
Conclusions
Although, both test and control sites showed favourable outcomes in relation to all the parameters but results obtained were better in the sites treated with Laser in terms hemostasis, wound healing, patient comfort and need for local infiltration. Within the limits of the study, it can be concluded that Laser appears to be a reliable alternative surgical tool to treat gingival overgrowth, offering advantages like bloodless field, sterilization of the surgical site, less postoperative pain with better healing and more patient comfort.