Introduction
Gingival recession can be defined as apical migration of gingival margin from the cementoenamel junction (CEJ) leading to exposure of root surface. According to the US National Survey, 88% of seniors (age 65 and over) and 50% of adults (18 to 64) presents with recession in one or more sites.1 It can be calculated by the distance between the CEJ to gingival margin. Aetiology of gingival recession is multifactorial such as presence of plaque and calculus, tooth malposition, high frenal attachment, improper tooth brushing, faulty restorations, smoking, tooth movement by orthodontic forces and recession after some periodontal surgeries by conventional/or chemicals methods etc. Gingival recession leads to exposure of tooth root which is further associated with increased chances of sensitivity problem, formation of plaque retentive area, root caries and aesthetic particularly in anterior aesthetic zone. In present era this becomes the major concern for the patient not only for facial aesthetic but personality as a whole.2
Non-surgical/Surgical management of gingival recession and its outcome can be affected by type of gingival recession (Miller’s Classification of Gingival Recession), 3 position of tooth, gingival phenotype, amount of attached gingiva and patient compliance. According to Lang and Löe, width of attached gingiva less than 2mm is inadequate for the maintenance of gingival health.4 Other studies suggested that <2mm or no keratinized gingiva is also adequate, if person is able to maintain strict oral hygiene.5, 6 The most predictable technique for increasing the zone of attached gingiva, improving the gingival phenotype and for gingival recession coverage is free gingival graft (FGG) by Bjorn, 1963.7
The aim of this paper is to present 3 cases for the management of gingival recession in mandibular anterior region and increasing the width of attached gingiva in Miller’s class II and III recession using free gingival graft.
Case Presentation
Case I
A -19 years old female reported to Dept. of Periodontology, Govt. College of Dentistry, Indore, with a chief complaint of receding gums in lower front tooth region. On examination patient was healthy with no systemic illness, had Miller’s Class II recession with #41, attachment loss of 5 mm and crowding in mandibular anterior region with less than 1 mm of amount of attached gingiva (Figure 1 a). Intraoral periapical radiograph (IOPA) with mandibular anterior region was done and patient was informed about the surgical correction of recession with FGG after phase 1.
Pre-surgical phase
Non-surgical phase along with scaling and root planning was conducted and patient was educated for plaque control. All necessary blood investigations were done in all the patient along with alginate impression was taken to prepare acrylic resin palatal plate after FGG procedure. Patient recall after 4 weeks for evaluation of gingival inflammation and procedure was planned.
Surgical phase
Medications given 1hr before the surgery (Cap. Amoxicillin 500mg, Tab. Ibuprofen 400mg), adequate local anaesthesia (2% lignocaine HCl with 1:80,000 adrenaline), recipient site prepared by giving one horizontal incision and two vertical incisions up to the vestibule from mesial and distal line angle of adjacent tooth with 15c blade, partial thickness flap is reflected and the frenum was released also vestibular deepening is done (Figure 1 b) , template to decide the size of the graft is prepared by aluminium foil (Figure 1 c), root surface was prepared by EDTA (RC Help, Prime Dental Products Pvt. Ltd) (Figure 1 d). Greater palatine nerve block was given, template placed in the palate (Figure 1 e), bleeding points are marked around the template margins (Figure 1 f), one parallel horizontal incision of 1.5mm depth was given 3-4 mm away from the gingival margin from the mesial line angle of the 1st premolar to the mesial line angle of 1st molar, two vertical incisions with help of tissue plier graft was hold and graft was separated from the underlying connective tissue and one horizontal incision was given in the apical end, graft was harvested (Figure 1 f),bleeding is controlled, fatty glandular tissue was removed, donor site was sutured with 3-0 braided silk suture (Mersilk, Ethicon, Johnson and Johnson Pvt. Ltd) (Figure 1 h), graft is closely adapted over the recipient with Oschenbein and circumferential sutures so there was no dead space left between the root surface and graft, by 5-0 monofilament suture (Prolene, Ethicon, Johnson and Johnson Pvt. Ltd) (Figure 1 I), periodontal dressing coe-pak is applied (Figure 1 J) and acrylic resin plate was given, analgesics and antibiotics for 5 days are given and chlorhexidine mouthwash 0.2% for 2 weeks, suture removal done after 14 days (Figure 1 K) follow up done after 1-month, 3-months and 6-months (Figure 1 L).
Figure 1
Gingival recession on lower incisors. B:Preparation of recipient site. C: Template preparation Root surface was prepared by EDTA. E: Template adaptation. F: Bleeding pointsmarked. G: Graft harvested. H:Donor site sutured. I: Graftclosely adapted over recipient site. J: Periodontal dressing applied. K: Follow up 1-month. L: Follow up 6-months

Case II
A 23yrs old female patient reported to Dept. of Periodontology, Govt. of Dentistry, Indore, with a complaint of sensitivity in mandibular anterior region. On examination patient was healthy with no systemic illness, has Miller’s Class III recession with #31 and #41 attachment loss 5mm and spacing in mandibular anterior region with no attached gingiva (Figure 2 a).
Medication given 1hr prior the surgery, adequate local anaesthesia (2% lignocaine HCl with 1:80,000 adrenaline), recipient site prepared by giving one horizontal incision and two vertical incisions up to the vestibule from mesial and distal line angle of adjacent tooth with 15c blade, partial thickness flap is reflected and the frenum was released also vestibular deepening is done (Figure 2 b), template to decide the size of the graft is prepared by aluminium foil (Figure 2 c). Greater palatine nerve block was given, template placed in the palate, bleeding points are marked around the template margins (Figure 2 d) and the graft was harvested (Figure 2 e), bleeding is controlled, fatty glandular tissue was removed, donor site was sutured with 3-0 braided silk suture (Figure 2 f), graft was closely adapted over the recipient with Oschenbein and circumferential sutures so there was no dead space left by 5-0 monofilament suture(Figure 2 g), periodontal dressing coe-pak is applied analgesics and antibiotics for 5 days are given and chlorhexidine mouthwash 0.2% for 2 weeks, suture removal done after 14 days, follow up. done after 1-month, 3-months and 6-months(Figure 2 h).
Case III
A 26 years old female reported to Dept. of Periodontology, Govt. of Dentistry, Indore, with a chief complaint of downward shifting of gums in front tooth region. On examination patient was healthy with no systemic illness, has Miller’s Class I recession with #41, attachment loss of 3mm and crowding in mandibular anterior region with 1mm of attached gingiva (Figure 3 a). Medication given 1hr prior the surgery, adequate local anaesthesia (2% lignocaine HCl with 1:80,000 adrenaline), recipient site prepared by giving one horizontal incision and two vertical incisions up to the vestibule from mesial and distal line angle of adjacent tooth with 15c blade, partial thickness flap is reflected and the frenum was released also vestibular deepening is done, template to decide the size of the graft is prepared by aluminium foil (Figure 3 b). Greater palatine nerve block was given, template placed in the palate, bleeding points are marked around the template margins and the graft was harvested (Figure 3 c), bleeding is controlled, fatty glandular tissue was removed, donor site was sutured with 3-0 braided silk suture, graft was closely adapted over the recipient with Oschenbein and circumferential sutures so there was no dead space left by 5-0 monofilament suture (Figure 3 d), periodontal dressing coe-pak is applied analgesics and antibiotics for 5 days are given and chlorhexidine mouthwash 0.2% for 2 weeks, suture removal done after 14 days, follow up done after 1-month , 3-months, 6-months of grafted site (Figure 3 e) & donor site (Figure 3 f).
Figure 3
A: Gingival recession on lower incisors. B: Preparation of recipient site. C: Graft harvested. D: Graft closely adapted over recipient site. E: Follow up 6-months. F: Doner site after 6 months
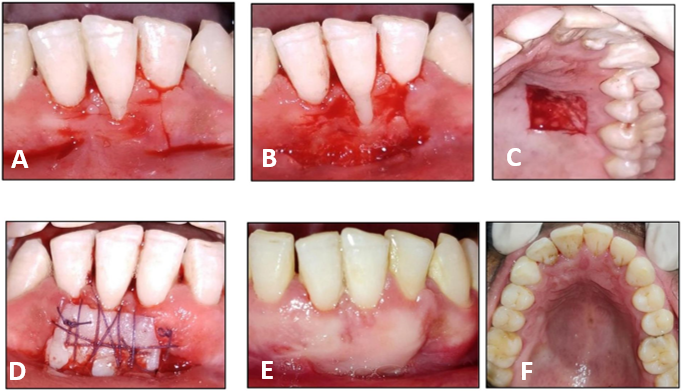
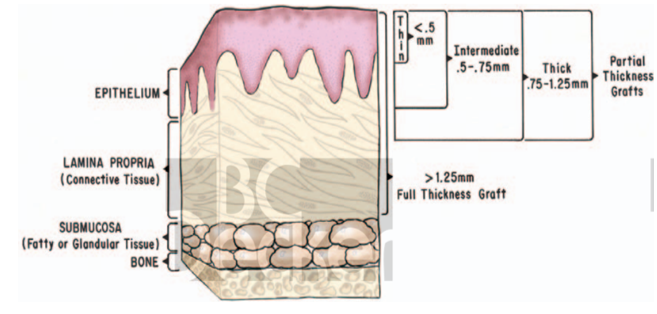
Figure 4
Thickness of graft. Cohen ES. Atlas of cosmetic and reconstructive periodontal surgery. PMPH-USA; 20078.
Discussion
In case I and III where Miller’s Class II and I gingival recession respectively, there is complete root coverage achieved and in case II Miller’s Class III type of gingival recession present 80% root coverage possible. According to cochrane systematic review mean root coverage in Millers Class I and II is 80.9% and complete root coverage 46.6%.9 After healing of graft root coverage is possible by creeping attachment i.e., coronal migration of epithelium.10 Healing takes place following adaptation of the graft a fibrin clot forms between graft and the underlying periosteal bed, which transport nutrients from the recipient area to connective tissue of the graft. Re-epithelization occurs from cells originating from lateral wound margins of epithelial ridges with in the graft in last half of the first post operative week with itself. After 72 hours proliferation of connective tissue begins and tenuous fibrous attachment formed between the graft and the recipient by the end of the first week a is seen. By 14th day the epithelium presents a near normal histologic thickness. Healing of a free gingival graft completed by reconstruction of the dentogingival junction coronal to the crest of the retained periosteum. There are different number of techniques for gingival recession coverage and for increasing the width of attached gingiva like coronally advanced flap, different types of pedicled grafts (lateral pedicle graft, double papilla graft), connective tissue graft, acellular dermal matrix (alloderm) which can be obtained by approved tissue bank but the long-term predictable result for recession coverage, increasing the width of attached gingiva and for ridge augmentation is free gingival graft. Sullivan and Atkins outlines need of different thickness of graft for different procedures, 0.5mm or 0.75mm (thin or intermediate graft) thickness ideal for increasing the width of attached gingiva as it has minimal amount of elastic fibre so it has less primary contraction. It goes 25-45% of secondary contraction (Ratertschak and colleagues, 1979; Ward, 1974)11, 12 due to cicatrization as it binds the graft to the underlying bed. 1.25mm or 2mm (thick or full thickness graft) can be used for root coverage procedure or ridge augmentation procedure it has higher primary contraction due to this it delays the revascularization as compared to less secondary contraction due to thicker lamina propria (Barsky and colleagues, 1964)8 also it creates the unesthetic patch. According to systematic review by SD Deo13 FGG best alternative for the treatment of gingival recession presents with inadequate width of attached gingiva and depth of vestibular fornix. Graft shrinkage is twofold more in vertical direction then horizontal, the mean vertical graft shrinkage ratio was 6.10±10.63 % (0 to 30 days), 5.16±8.70 % (30 to 90 days), 10.87± 13.56 % (0 to 90 days).14 Main disadvantage of FGG is unesthetic appearance, two donor site, donor site morbidity, age and limitation of patient systemic condition.

