Introduction
Periodontitis is an infectious disease caused by gram-negative anaerobic microorganisms in the dental biofilm, resulting in inflammation within the supporting structures of the tooth, leading to progressive attachment and bone loss, characterized by pocket formation and recession. Periodontitis leads to epithelial proliferation and migration, which results in the chronic release of inflammatory cytokines, prostaglandins, growth factors, and enzymes, all of which are closely associated with the development of cancer.1
Ample research evidence has suggested that chronic infections and inflammation are related with increased risk of cancer. The role of bacterial and viral infections in carcinogenesis has also been highlighted.1
There has been a notable interest in understanding the role of periodontitis and risk of cancer, due to the advancement of research on human microbiome and the advent of animal models, enabling the assessment of the effect of periodontal pathogens on immune response.2
Cancer Ascertainment
Incidence of cancers were ascertained from 1987 to 2012 through linkage with state cancer registries in Minnesota, North Carolina, Maryland, And Mississippi, and supplemented by abstraction of medical records and hospital discharge codes for self-reported cases (supplementary methods, available online). Cancer deaths were obtained from death certificates where cancer was the underlying cause of death.3 From enrolment through 2012, 4107 first primary cancer cases and 1661 cancer deaths were noted. Out of which, 3748 were first primary cancers and 1332 were cancer deaths that occurred after visit 4. Of these, 1648 and 547, respectively, occurred among those in the study population over a mean of 14.7 years of follow-up.3
Evidence fir association
Individuals diagnosed with cancer often refrain from regular brushing of teeth and usage of cleaning aids. This can be attributed to the fact that they suffer from depression, which is often not diagnosed and treated. As the therapy starts, patients may undergo chemotherapy /radiotherapy, which have negative affect on oral hygiene habits. Poor maintenance of oral hygiene along with a depressed state of mind, increases the likelihood of gingival bleeding and burden of periodontal infection.2, 4, 5, 6 The association between poor oral health and cancer has been substantiated in several studies. Compromised oral health was observed in nasopharyngeal carcinoma survivors (1-4 years after radiotherapy).7, 8
A study on 73 patients diagnosed with acute myeloid leukemia (AML), pointed that about three-quarters of the patients with acute myeloid leukemia showed poor or fair oral hygiene.9
A prospective study, evaluated the link between tooth loss and the risk of developing esophageal squamous cell carcinoma, gastric cardia adenocarcinoma or gastric non-cardia adenocarcinoma in a 28,868-person cohort, and was followed prospectively for 5.25 years. The analytic cohort included 620 esophagus, 431 gastric cardia, and 102 gastric non-cardia cancer cases. In this cohort study, tooth loss increased the risk of developing upper gastrointestinal cancer. It was stated that this may be related to alterations in the oral bacterial flora and subsequent increases in the in‑vivo production of carcinogens, such as, nitrosamines.10
Recent study conducted JNCI National CANCER INST 2018 on assessing periodontal disease assessed using clinical dental measurement and cancer risk in ARIC study. This study gave additional evidence that cancer risk, especially for lung and colorectal cancer, increases in individuals with periodontitis. Additional research is essential to understand cancer site–specific and racial differences in findings.11
The relationship between chronic and oral cancer periodontitis
Genetic predisposition, presence of premalignant lesions, effect of environmental or carcinogenic factors, such as tobacco and alcohol consumption, are some of the risk factors suggested as risk factors for the incidence of oral squamous cell carcinoma. The role of infection and inflammation with human papilloma virus has also been noted in oropharyngeal carcinomas10 along with the role of chronic periodontitis in the oral cancer development.11, 12 In a recent study, bone loss, a clinical sign of chronic periodontitis was indicated as an independent risk factor for the development of cancer in the oral cavity.13
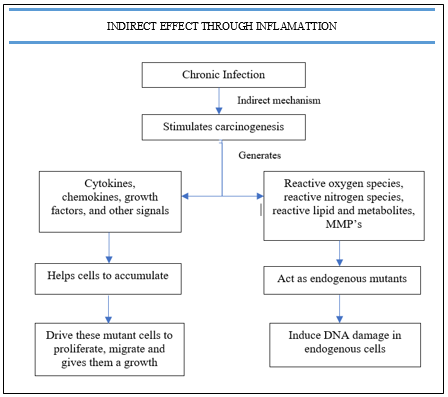
The research concentrated on the different types of cancer , their association with the inflammation and the pathophysiological mechanisms behind malignant cellular transformation.14, 15 A key factor in inflammation linked with cancer is NF-κb transcription factor, a basic regulator of the innate inflammation and immunity through an activated expression of inflammatory biomarkers namely cytokines, chemokines, adhesion molecules, proteolytic enzymes, angiogenic factors and a wide spectrum of toxic metabolic cellular substances. It therefore plays an important role in the inflammatory reaction in chronic periodontitis .as well as a potent endogenous tumor promoter.10
Furthermore, inflammation, despite the underlying etiology, can predispose to cancer development,16 thereby explaining the malignant transformation of the oral epithelial cells. This may be an adverse effect of an immune response via the release of activated t-cells substances, such as cytokines IL-1, IL-8 and TNF-α.17
The biological plausibility of the association between periodontitis and cancer may be interpreted on the basis of the following mechanisms,1
Periodontal disease - facilitating enhanced carcinogen penetration (smoking and alcohol , disrupt the mucosal barrier
Chronic inflammatory response causes a chronic diffuse hyperplasia of the epithelial cells (increased cell load in the blood vessels and the connective) indicated as a common precursor of the intraepithelial neoplasia
Immunosuppression is a common mechanism that leads to periodontal disease and oral cancer
Viruses such as human papilloma virus and herpes simplex virus1 or the fungus Candida albicans have been isolated in both oral cancer and periodontal disease
In patients with poor oral hygiene, bacterial overload can lead to an increase in the proportion of metabolites with a potential carcinogenic effect
In dizygotic twins, who share common genetic risk factors, periodontal disease is a risk factor for cancer development, whereas in monozygotic twins this association was significantly impaired.18
Recent studies reported that some viruses such as human papilloma, cytomegalo virus and Epstein Barr present in periodontal pockets and in dental plaque,19, 20 are implicated in oral cancer etiology.
Cacteria and viruses in associated cancer
Several studies have established the role of helicobacter pylori in development of gastric cancer and chlamydia pneumonia infection with lung cancer. Streptococcus bovis infection was found to be associated with colon cancer while other bacteria such as salmonella typhi was linked with gall bladder cancer and hepatobiliary carcinoma.21
Epstein-Barr virus is believed to be associated with Burkitt lymphoma, Hodgkin lymphoma, nasopharyngeal carcinoma, and stomach cancer. Human herpes 8 is associated with kaposi sarcoma. The hepatitis b virus has its involvement in liver cancer and human t-lymphocytic virus with adult T-cell leukemia. The cytomegalovirus is associated with cancer of the salivary gland and prostate. The human papilloma virus is linked with cancer of the cervix, vulva, penis, and anus.22, 23, 24, 25, 13, 3, 26 It has been suggested that herpes viruses might impair local host defense by disrupting the protective epithelial barrier by lysing the epithelial cells, or by altering the expression of cell surface receptor molecules. Human papilloma viruses, cause characteristic cytopathic effects (koilocytosis), a proliferation of epithelial cells. It is known that proliferation and migration of the junctional epithelium are a major hallmark of periodontal breakdown, these known biological effects of HPV might provide a link between viral infection and periodontal disease. Productive infection by HPV is tightly linked to the differentiation program of the host keratinocyte. Following entry into the basal epithelial cells, HPV genomes are established as autonomous replicating extra-chromosomal elements and a low level of HPV expression occurs. Upon differentiation of infected cells, productive replication and expression of capsiden coding genes (L1 and L2) is induced, resulting in the production and assembly of mature viral particles. Theoretically, the junctional epithelium attached to the tooth surface appears to fully serve the cellular functions required by HPV. It has a basal cell-like phenotype and does not differentiate. The basal cells are exfoliated through the gingival crevice before differentiation occurs.
Biologival Mecganism
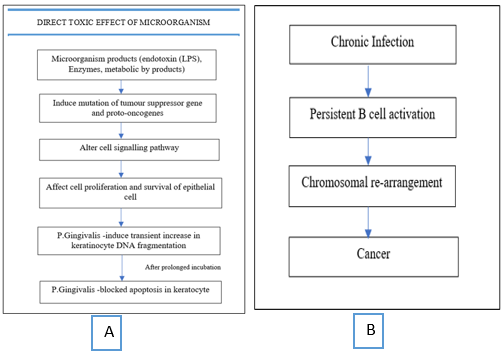
Figure 1
A: Direct Toxic Effect of MicroorganismP. Gingivalis-major periodontal Pathogen, capable of invading Epithelial cell Figure 1B: Example of Direct Toxic Effect of Microorganism. Direct Bacterial stimuli – in association between Helicobacter pylori and primary B cell gastric lymphoma
Another link was explained between periodontal disease and risk of pancreatic cancer. The carcinogenic compounds, namely, nitrosamines and bacteria, react with the digestive chemicals in the gut to create conditions that favour the development of pancreatic cancer.11
The shared genetic factors may partially explain the association between cancer and periodontal disease, in the case of digestive tract cancer.26 There are many other risk factors modifying the development of cancer. Smoking and usage of smokeless tobacco have also proved to be the main risk factors associated with cancer development.26 The strength of association is higher in a past smoker or a ‘never smoker’ when compared to current smokers. Alcoholism along with smoking gives an additive effect in carcinogenesis. Diet, age, gender, and family history also play an important role in carcinogenesis.26
Conclusion
Summarizing the review, the studies done by various authors throw light on the fact that compromised oral health may prove a risk factor for carcinogenesis. The association between periodontal disease and oral and/or oropharyngeal cancer may have implications for public health in preventive measures and for the patients who might experience major improvements in the complications of cancer and its treatment. An association between periodontal disease and cancer may lead us to consider patients with periodontitis as population at risk for developing oral/oropharyngeal cancer. In considering all the studies it is obvious that there is a need for further investigation.