Introduction
The American Academy of Periodontology defined root amputation as a process by which one or more of the roots of a tooth are removed at the level of furcation while leaving the crown and remaining roots in function. Root amputation otherwise called as radisection or root resection can be distinguished from crown resection (CR) procedure, by the former being defined as a process including amputation at the level of the cementoenamel junction with intact coronal portion. But on the other hand, “crown resection” includes hemisection, trisection, or bicuspidization of the crown in a multirooted tooth, which is traversed through the furcation in a way that both the root and the associated portion of the crown may be removed or retained. 1, 2
Indications for root amputation therapy include: teeth with periodontal problems, endodontic problems, root fractures, and prosthetic problems. In endodontic complications such as root fracture, file fracture, root perforation, deep subgingival caries, radisection could be a boon if the teeth are of high strategic value or when all other approaches to save the diseased tooth have failed. During such times of complications, a choice between preservation and extraction followed by replacement of lost tooth structure has to be made. Root resection is one treatment option for preserving molars with furcation involvement.
Early in 1960’s, the therapy involving root resection was right on the cutting edge in periodontics and endodontics. ‘Hiat’ and ‘Amen’ contributed in the quest for salvaging teeth by comprehensively describing the indications and techniques for root amputation. In reality ‘G.V Black’ described almost the same methods in the nineteenth century and by ‘Sharp’ in 1920.
Weine” has listed the following indications for tooth resection: 3
Severe vertical bone loss involving only one root of multi-rooted teeth.
Through and through furcation destruction.
Unfavorable proximity of roots of adjacent teeth, preventing adequate hygiene maintenance interproximal areas.
Severe root exposure due to dehiscence.
In case of periodontally diseased molars, root amputation has been found to be a viable option. In this case the bone resorption occurs mainly due to failure in RCT, which was secondarily affected periodontally. Careful evaluation of the radiographs revealed the presence of a furcation defect, bone loss and a periapical radiolucency. The remaining structures were found to be normal. The root amputation therapy was selected for this case as it ideally had the disease involving a single root with the remaining tooth structure stable with adequate bone support.
Case Report
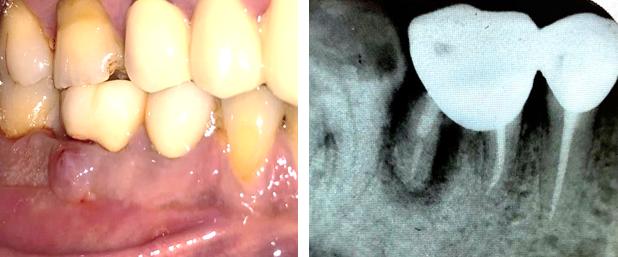
A 45 year old male patient reported to the department with the chief complaint of pain, food impaction, and pus discharge in the lower right posterior tooth .On clinical examination, a metal ceramic bridge was present connecting 46 and 45 and , abscess was present irt 46. A diagnostic radiograph reveals that 46 and 45 was root canal treated but the distal root of 46 was underobturated. Severe vertical bone loss was evident surrounding the distal root of 46 and involves the furcation area. The bone support of mesial root was completely intact. Tooth was tender on percussion with a deep periodontal pocket of 9 –10 mm on distal root of 46 region. Interproximal bone loss was seen between 46 and 47. Treatment options included extraction of 46 alone by preserving 45 followed by placement of implant later on 46, new fixed partial denture including 47 or removable partial denture. Patient did not wish to have the tooth removed, so conservative treatment option of root amputation and its pros and cons was explained. Patient happily opted the choice which included root amputation of the distal root of 46 by preserving the FPD.
Procedure
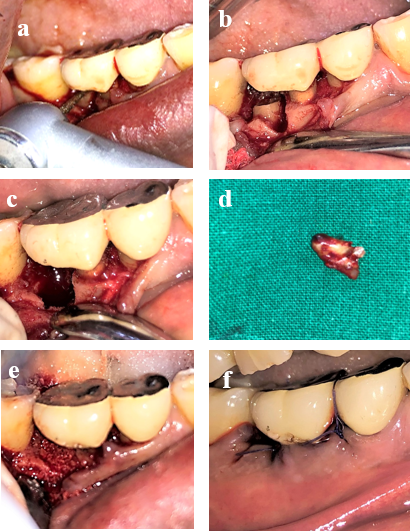
All procedures were performed under strict sterile conditions. A phase I therapy including scaling and root planning was performed and the pus drainage was done. Local anaesthesia (lidocaine 2% with 1:80,000 epinephrine) was administered. After achieving adequate local anesthesia a full-thickness mucoperiosteal flap by means of crevicular incisions was raised both on the buccal as well as lingual sides to expose the margins of the bone defect. Upon reflection of the flap, the bony defect along the distal root became quite evident. A rotary motor utilizing straight end plain fissure carbide bur with irrigation was used to resect the distal root, apical to CEJ. The cut was made from apical to the contact point of the tooth, through the tooth, and to the facial and distal orifices of the furcation. A fine probe was passed through the cut to ensure separation. After completion of the sectioning, the root was elevated from its socket with a periosteal elevator and removed. The distal root was extracted carefully. The surrounding bone around the next teeth was preserved to prevent bone resorption. After curetting and elimination of the granulation tissue from the socket and removal of the tissue tags from the flap; thorough root planing of the mesial root was performed. After complete debridement, the open distal root orifice was sealed using bone graft (osseograft) and PRF. The flap was sutured using 3-0 braided black silk sutures (Ethicon US, LLC, U.S) and periodontal pack was placed. Amoxicillin was prescribed for 5 days (Amox 500 mg/tid) and was asked to continue with 0.2% chlorhexidine rinse.
The sutures were removed after 15 days. Betadine and saline irrigation done. The surgical site exhibited good healing. No postoperative complications were noticed. There was no swelling or any exaggerated pain or discomfort as reported by the patient. The soft tissue had collapsed in the distal aspect leaving a space of more than 3 mm apical to the crown, making it self-cleansable. Oral hygiene instructions and touch to teach brushing technique was advised. The patient was advised to use a interproximal brush to keep it clean. Radiographically some evidence of bone formation was noticed distal to mesial root during one month review
The patient was again evaluated after six months. The surgical site showed no sign of inflammation.
The resected tooth exhibited absolutely no mobility. Soft tissue appears to be firm and healthy.
The patient reported after one year and the resected tooth exhibited no sign of gingival inflammation and shows excellent healing. Soft tissue covered the interdental area. No food impaction was present. The intraoral periapical radiograph depicted clear picture of regenerated bone in relation to the mesial root and on the extracted socket of 46.
Discussion
Root amputation, or resection, is a periodontal surgical technique used to maintain the healthy portion of a molar that has a diseased or damaged root (upper molars have three roots, and lower molars have two roots). If a single root get infected, the surrounding gum tissue may also become infected, which leads to the formation of pockets which result in the bacterial growth and plaque accumulation.
Rot resection is also performed in conditions where roots are so close together so that that the plaque removal and root planing cannot be performed, root amputation can be used to make room between molars to allow for manageable, non-surgical periodontal treatment to be performed.4
A tooth is considered as a good candidate for a root amputation, when the root that has been previously treated by a root canal treatment is suffering from embedded bacteria, severe bone loss due to infection or fracture, or decay in a concentrated area. If the root is suffering from decay, the rest of the roots need to have sufficient amount of bone to support the tooth in question in order to perform the root amputation. That means if the issue is only impacting on one root, and the remaining tooth structure is healthy, a root amputation can be performed successfully to save the tooth.4
If left untreated, the infection or decay can spread to the surrounding areas and result in the loss of tooth. This jeopardizes the stability not only of the tooth with the problem, but the surrounding teeth as well. Eventually health of the whole tooth will be compromised, which result in the extraction of the tooth. Removal of one root can help to save the tooth and prevents you from the need of extraction and replacement with a partial, bridge, or implant.
Root amputated molars demonstrated the highest degree of failure when they were long standing terminal abutments. It has been reported that molars with bone support of more than 50% of the remaining roots at the time of root amputation had a significantly higher survival rate compared with that of molars with less than 50% bone support. Occlusion should be evaluated, and the root resected tooth should receive full coverage if not already present to prevent a vertical root fractures, which is one of the most common complications following root amputation procedures
Eventhough hemisection is more preferable on mandibular molars than radisection, due to the patient inconvenience to repeat the FPD and due to the presence of adequate bone support on mesial root of 46 here we opted radisection as a treatment of choice. One year follow up shows a good prognosis with no mobility, no food impaction, healthy gingiva, and favourable amount of bone regeneration. For a better prognosis good post-operative oral hygiene should be maintained in future also, especially in the area of root amputation.
Conclusion
In treatment planning one should always remember that our goal should be preservation of what remains intact. In accordance with the current case report, root amputation can be viewed as a valid treatment option to eliminate the diseased root so as to allow the remaining healthy tooth to survive.