Introduction
Oral squamous cell carcinoma (OSCC) constitutes more than 90% of the carcinoma of oral cavity. It is the sixth most common cancer affecting males and tenth most common cancer affecting females worldwide by constituting a major health problem leading to death.1 Oral Squamous Cell Carcinoma occurs in oral cavity and oropharynx which occurs due to many etiological factors yet smoking and alcohol being the most common risk factor. The most common site of oral squamous cell carcinoma is lateral surface of the tongue, floor of the mouth and the least common site are gingiva, buccal mucosa and soft palate.2 Gingival squamous cell carcinoma is rare and comprises only of 10% of oral squamous cell carcinoma. Diagnosis of gingival SCC is challenging because it is often misdiagnosed as chronic periodontitis, gingival enlargement, or other benign tumours. Early diagnosis and proper treatment of any gingival lesion is of utmost importance and thereby necessary for good prognosis.
Case Report
A 70 years old male patient reported to the Department of Periodontology and Oral Implantology with a chief complaint of pain and swelling in the upper left back gum region for past 2 months and there was slight bleeding on stimulation and burning sensation and there was no other relevant history.
The patient is a known hypertensive for past 20 years and diabetic for past 15 years and is under medication for the same. Social history was negative for contributing factors such as tobacco, alcohol, or chemical exposure. There was no significant family history. There was no history of weight loss or appetite over the last few months.
On general physical examination, the patient was well built and nourished. All the vital signs were within the normal limits. Extraoral examination revealed no facial asymmetry and on palpation, left submandibular lymph node was palpable which was fixed, hard and non-tender.
The intra oral examination revealed a swelling on the buccal gingiva of teeth 24 and 25 which extends from mesial aspect of 24 to distal aspect of 25, superiorly from the buccal vestibule and inferiorly terminating on the marginal gingiva of 24 and 25 and measuring approximately 2cm x 2cm. (Figure 1: Initial visit) The lesion appears erythematous with speckled non scrapable white patches and the surface was slightly eroded and ulcerated. The margins of the gingival lesion were well-defined with raised edges. The gingival swelling was soft to firm on palpation with a sessile base.
Periodontal examination revealed bleeding on probing with no exudation and tenderness on palpation in relation to 24, 25, 26. Pocket probing depth ranging from 5 to 7 mm was present in relation to teeth 24,25,26. The teeth were attrited and not mobile. There was no tenderness on lateral and vertical percussion on teeth 24 and 25. The gingiva and alveolar mucosa at the adjacent sites were clinically normal with minimal plaque accumulation. A provisional diagnosis was carried out as Pyogenic Granuloma.
Intraoral periapical radiographic examination revealed moderate horizontal bone loss in relation to teeth 24 and 25 and there was no bony involvement of the lesion.
Differential Diagnosis of erosive lichen planus, verrucous carcinoma, deep fungal infection, chronic traumatic ulcer, squamous cell carcinoma was given.
Routine periodontal phase I therapy including scaling and root planning was performed in relation to teeth 24 and 25 with systemic antibiotics. The patient was advised to take amoxicillin 500 mg three times a day, diclofenac 50 mg+paracetamol 500 mg twice daily for 5 days and chlorhexidine mouthwash twice daily for 7 days.
On recall after 7 days, the patient reported with severe pain and discomfort on the left side of the maxilla and Clinical examination revealed an extensive erythematous and granular appearing hyperplastic tissue on the facial aspect of 24 and 25. (Figure 2: After scaling and root planing) The lesion was tender on palpation. Diclofenac 50 mg+paracetamol 500 mg three times a day for 3 days was prescribed and incisional biopsy was planned.
Incisional biopsy was performed on the left maxillary buccal gingiva (2x2x2cm) in relation to teeth 24 and 25 the next day, stored in formalin and the specimen is sent for histopathological examination. (Figure 3: Excision of gingival lesion; Figure 4: Excised tissue) One week after incisional biopsy, the intraoral picture revealed incomplete healing of the gingival tissue. (Figure 5 : Review after one week)
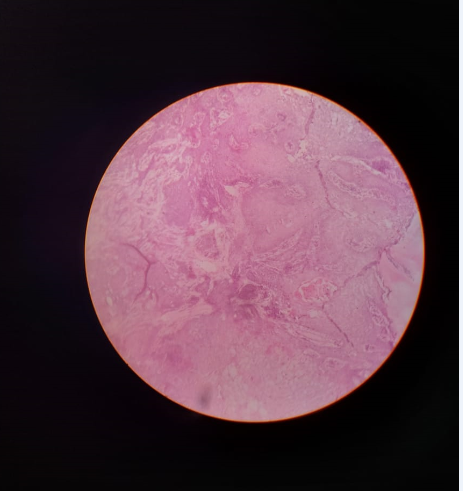
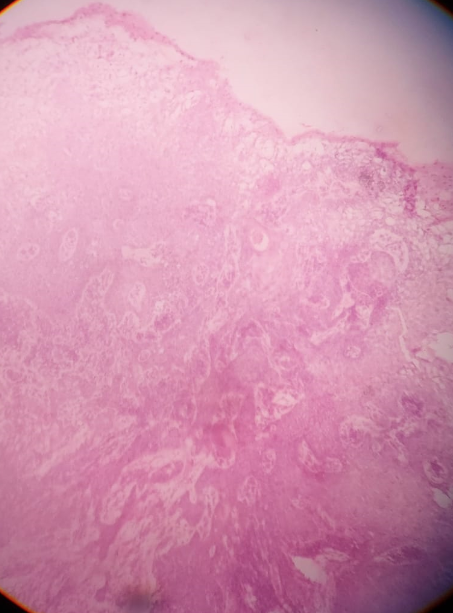
On Histopathological analysis, severely dysplastic stratified squamous surface epithelium exhibiting elongated rete ridges was seen invading into connective tissue in the form of islands and cords in varying size. (Figure 6: Histopathology showing epithelial dysplasia) Cells show epithelial dysplastic features like nuclear hyperchromatism, prominent nucleoli and keratin pearl formation. Mitosis was seen and connective tissue showed a dense lymphoplasmacytic infiltrate, giant cell, and engorged blood vessel. (Figure 7: Histopathology showing keratin pearls) The biopsy report confirmed that the gingival lesion was well‑differentiated SCC.
Patient was advised to take CT, and the reports showed minimally suspicious ill-defined soft tissue thickening in relation to gingivobuccal sulcus of maxilla adjoining molar region on the left side measuring about 2cm and few small sub centimeter deep cervical lymph nodes were also seen. CT chest did not reveal any metastasis from the lungs. The patient was referred to the department of oncology for further needful management.
Discussion
Globally, oral cancer is the sixth most common malignancy and squamous cell carcinoma is the most common malignant tumour of oral cavity followed by lymphoma and mucoepidermoid carcinoma. Squamous cell carcinoma is an epithelial tumour and occurs frequently in tongue, buccal mucosa, floor of the mouth, followed by lips, alveolus, gingiva and palate. The site predilection is due to the thin, non-keratinizing mucosa of those regions which are less resistant and more prone to carcinogens. Gingival squamous cell carcinoma is an aggressive disease accounting for <10% of all intra oral squamous cell carcinoma.3 The most important aspect of gingival SCC is that it has a higher risk of causing metastasis and consequent death with less survival rate.
The main etiological factors for squamous cell carcinoma are smoking, chewable tobacco and alcohol. Other factors include syphilis, phenol usage, ultraviolet radiation, iron deficiency, Candidal infections, human papilloma virus, Epstein-barr virus which have very minor role.4 In a study by Simiantonaki et al pro-inflammatory stimuli from bacterial lipopolysaccharide plays a major role in tumour metastasis and tumor cell-mediated induction of endothelial cell adhesion. But gingival squamous cell carcinoma does not have a strong correlation with usual risk factors such as tobacco or alcohol.5 Many studies shows that squamous cell carcinoma has age predilection of 60 years and above. This carcinoma more frequently involves mandible than maxilla and targeting females of older age group.6
Gingival squamous cell carcinoma is often symptomless and the initially presents as an intraoral mass or swelling, unhealing ulcer and extraction wounds, pain, ill-fitting dentures, mobility of teeth. These tumours commonly resemble inflammatory lesions of the periodontium such as gingivitis, periodontitis, pyogenic granuloma or conditions like candidiasis, verruciform xanthoma. The lesions are often misdiagnosed as advanced periodontitis at an early stage as it is accompanied with minimal pain and discomfort.7
Cady and Caplin in their 20 years survey observed that 60% of patients were initially seen by the dentists and were immediately diagnosed and referred for appropriate therapy.7 In their study of 595 patients with oral cancer, 8% patients had gingival squamous cell carcinoma, and 52% patients consulted the dentist as their initial professional contact. Gingival squamous cell carcinoma is often misdiagnosed as oral enlargements which might worsen the prognosis. A simple oral prophylaxis, curettage, extraction can increase the severity of the disease by embedding the cancer cells into the circulation and further increases the chances of metastasis the tumour.
The treatment of squamous cell carcinoma of the oral cavity depends on the patient and tumour factors. Nutritional status, associated diseases, co-morbidities, oral behaviours are some of the patient related factors and tumour factors are its size, site, histology and biological behaviours. Mostly, oral cancers are treated with chemotherapy or surgery or radiation or combination therapy. Surgery is indicated in typical smaller lesions whereas radiation therapy is preferred in case of recurrence. Early invasion of the periosteum and bone is seen in gingival squamous cell carcinoma because of its proximity which may occasionally, rapidly infiltrate and extend along the periodontal ligament and thus destroying the alveolar bone.8
The clinical extent of the tumour and histological subtype determines the prognosis of gingival squamous cell carcinomas. Prognosis is less in cases with advanced maxillary gingival squamous cell carcinoma as it exhibits aggressive regional metastasis to skull base which might become inoperable. Favourable prognosis is seen in cases of well differentiated squamous cell carcinoma. Also, the lesion of size <1cm are easier to treat and have a long-term prognosis. If the neoplasm is small and localized then the 5-year survival rate is said to be 60-70%; whereas in case of cervical nodal metastasis, the survival rate is only around 25%.9 So, the most important prognostic indicator is the clinical stage of disease. Gingival squamous cell carcinoma shows cervical metastasis is more than one third of the cases, so early diagnosis is a key factor in the treatment of SCC.
Newer diagnostic methods like immunohistochemistry offers easy identification through various markers. In a study by Kuratomi et al, markers like Mina 53 and Ki67 was similar in both normal gingival and dysplastic tissue. However, the expression of Ki67 was more in cases of well differentiated gingival squamous cell carcinoma. Nuclear proliferating markers like AgNOR and p53 is used for the detection of oral squamous cell carcinoma. It is observed that there is an increasing trend in AgNOR and p53 expression in relation to progressing histological grading of oral squamous cell carcinoma.10
In this case, the patient did not have any risk factors associated with the neoplasm and also the patient age was 70 years which gives a positive correlation between age and squamous cell carcinoma. There was also no sex and site predilection in this case for gingival squamous cell carcinoma which makes it as a challenging case.
Conclusion
Oral squamous cell carcinoma is highly fatal. Inspite of novel and significant advancement in diagnosis and treatment planning, the 5-year survival rate remains very low. In this case, even though the patient presented with independent risk predictor like male gender, late clinical stage at presentation and advanced age, early detection and necessary treatment will help in improving survival rate of the patient.