Introduction
Scientific rationale
Primary closure is the most important step following tooth extraction.1 Various techniques of closure have been advocated in the past. Knowledge about the extraction healing process and the preservation of the alveolar socket is essential in treatment planning.2, 3, 4 Socket preservation procedures were performed in order to preserve the hard and soft tissue volume, which can be partially lost after tooth removal.2, 5
Cut back technique was firstly introduced by Corn in 1964.6 He advised that giving the cut back incision reduces the muscle tension on the flap and allows free advancement of the flap in coronal direction causing complete closure.7 Primary closure using cut back technique also helps in preserving the bone graft in socket and to seal it in their desired position.
Aim
To compare and evaluate the difference in healing outcome of cut back incision and without cut back incision technique in subjects of either sex between 18-65 years undergoing extraction for socket preservation at baseline, 1 week and 4 weeks postoperatively.
Objective
To assess the healing outcome with and without cut back incision technique in subjects of either sex between 18-65 years undergoing extraction for socket preservation at baseline, 1 week and 4 weeks post-operatively with respect to:
Materials and Methods
Trial design
This study was Parallel arm, single blinded randomized controlled trial consisting of allocation ratio as 1:1. The study was performed after the approval of Institutional ethical committee (YMTDCH/IEC/2020/118) board at YMT Dental College and Hospital, Navi Mumbai and the study was registered at the Clinical Trial Registry-India (REF/2021/04/043237) with the Helsinki Declaration of 1975 that was revised in 2000.
Participants
Inclusion criteria
Systemically healthy subjects of either sex between 18-65 years
Width of keratinized tissue >2mm
Anterior and premolar teeth indicated for extraction
Teeth with endo-perio lesions indicated for extractions
Teeth suffering from mild (up to 15% of root length or ≥2mm and ≥3 mm) to moderate (16% to 30% or >3mm and ≤ 5mm) radiographic bone loss will be included.
Exclusion criteria
Subjects with history of antibiotic and/or anti-inflammatory drugs within previous three months
Subjects with history of any periodontal therapy in the past 6 months
Severe periodontitis cases
Subjects with systemic conditions modifying the inflammatory response
Smokers & Tobacco chewers
Pregnancy or lactation
Uncooperative subjects
Interventions
Method of data collection
Selection of cases with extraction of either sex within the age range of 18-65 years.
The subjects undergoing this study had to sign an informed consent form after being informed about the nature of the study in detail and in a language best understood by them.
A detailed case history was recorded, and the surgical procedures were performed under local anaesthesia respectively.
Phase I therapy (scaling and root planing) was carried out and oral hygiene instructions were given.
Surgical procedure
In both the groups surgery was performed by the same surgeon.
In Group 1, patient was scrubbed and draped in all aseptic conditions.
Local infiltration using lignocaine with adrenaline (1: 80,000) was administered.
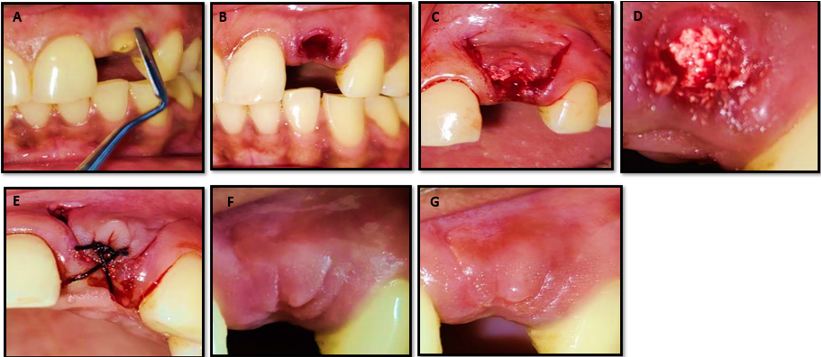
Atraumatic extraction (Figure 1:A&B) was carried out using periotome and luxators, socket was curetted well, debrided and betadine irrigation was performed.
Using a 15-no. blade a full thickness envelope flap was raised around the socket with two vertical releasing incisions, anterior and posterior. (Figure 1:C)
The releasing incisions extended 3 - 4 mm upto the mucogingival junction and were followed by two back cut incisions at the base. This was followed by two horizontal incisions at 45 to 60 degree angulation towards the centre of flap. (Figure 1:C)
After which the socket was grafted with bone graft (allograft + alloplast). (Figure 1:D)
Once the flap was elevated, it was advanced to obtain primary closure over the open wound of the socket.
After checking flap mobility, advancement of the flap was carried out and flap was moved coronally and sutured with 3-0 silk in the new location as it was designed before in order to obtain tension free primary closure.(Figure 1:E)
In Group 2, patient was scrubbed and draped in all aseptic conditions.
Local infiltration using lignocaine with adrenaline (1: 80,000) was administered.
Atraumatic extraction was carried out using periotome and luxators, socket was curetted well, debrided and betadine irrigation was performed. (Figure 2:A&B)
-
After extraction, the socket was grafted with bone graft (Figure 2:C) and sutured with 3-0 silk in order to obtain closure. (Figure 2:D)
Post-operative instructions were given to the patient.
Patient was instructed to apply ice intermittently over the operated area for 10-20 minutes after surgery.
Patient was advised to consume soft semisolid or finely minced food.
Patient was asked to avoid hot, hard and spicy food stuff.
Patient was restricted to brush over the operated area.
Patient was prescribed antibiotic and analgesic therapy, consisting of 500mg of Cap.Amoxicillin, which commenced from 1 day before surgery and thrice a day, for 5 days post operatively; Tab Ibuprofen 400 mg to be taken thrice a day for 3 days after surgery and chlorhexidine spray to be used 3 times daily for 15 days.
Mouthwash containing 0.2% Chlorhexidine, 10ml twice daily for 15 days was prescribed to maintain the oral hygiene.
Group 1: Cutback Incision Technique
Figure 1
A): Atraumatic Extraction using Periotome with 21; B): Extracted Socket w.r.t 21; C): Two Vertical Releasing incisions followed by Two Cutback Incision at 45° angle towards the midline; D): Socket Preservation done using a mixture of Allograft+ Alloplast; E): Advancement of the flap followed by primary closure with 3-0 Silk Suture; F): Post-operative Follow up at 1 week; G): Post-operative Follow up at 4 weeks
Group 2: Without Cutback Incision Technique
Figure 2
A): Root piece w.r.t 45; B): Atraumatic Extraction Performed and Extracted socket w.r.t 45; C): Socket Preservation done using a mixture of Allograft+ Alloplast; D): Primary closure with 3-0 Silk Suture; E): Post-operative Follow up at 1 week; F): Post-operative Follow up at 4 weeks.
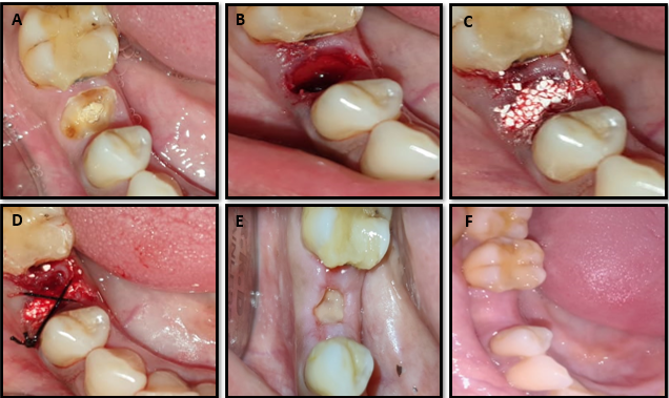
Table 1
Primary Healing
|
|
Mean |
SD |
Minimum |
Maximum |
Median |
Mean rank |
Chi square value |
p value of Friedman Test |
|
Baseline |
1.00 |
.000 |
1 |
1 |
1.00 |
1.81 |
12.000 |
0.002** |
|
1week |
1.38 |
.500 |
1 |
2 |
1.00 |
2.38 |
||
|
4weeks |
1.00 |
.000 |
1 |
1 |
1.00 |
1.81 |
Table 2
Pain on Vas Scale
|
|
Mean |
SD |
Minimum |
Maximum |
Median |
Mean rank |
Chi square value |
p value of Friedman Test |
|
Baseline |
.81 |
.750 |
0 |
2 |
1.00 |
1.72 |
21.138 |
0.000** |
|
1week |
2.19 |
.834 |
1 |
3 |
2.00 |
2.88 |
||
|
4weeks |
.56 |
.512 |
0 |
1 |
1.00 |
1.41 |
Table 3
Keratinized Gingiva Width
[i] Table 3 (Keratinized Gingiva Width)there was a statistically non-significant difference seen for the values between the time intervals (p>0.05)
Table 4
Primary Healing
|
|
Mean |
SD |
Minimum |
Maximum |
Median |
Mean rank |
Chi square value |
p value of Friedman Test |
|
Baseline |
1.00 |
.000 |
1 |
1 |
1.00 |
1.69 |
20.000 |
0.000** |
|
1week |
1.75 |
.683 |
1 |
3 |
2.00 |
2.63 |
||
|
4weeks |
1.00 |
.000 |
1 |
1 |
1.00 |
1.69 |
Table 5
Pain on Vas Scale
|
|
Mean |
SD |
Minimum |
Maximum |
Median |
Mean rank |
Chi square value |
p value of Friedman Test |
|
Baseline |
.38 |
.619 |
0 |
2 |
.00 |
1.47 |
26.627 |
0.000** |
|
1week |
3.31 |
1.250 |
1 |
5 |
3.00 |
2.94 |
||
|
4weeks |
.56 |
1.031 |
0 |
3 |
.00 |
1.59 |
Table 6
Keratinized Gingiva Width
[i] Table 6 (Keratinized Gingiva Width) there was a statistically non-significant difference seen for the values between the time intervals(p>0.05).
Table 7
Inter Group Comparison (N=16 Per Group)
[i] Table 7 summarises the significant inter group comparisons between the outcome variables related to Group 1 and Group 2. which shows that there was a statistically highly significant difference seen for the valuesbetween the groups (p<0.01) for Pain on VAS Scale and KGW 1week with higher values in group 2 and non significant results were seen in both groups at 4weeks.
Outcomes
The primary outcomes were to check the primary closure percentage by evaluating healing using healing index given by Huang et al in the year 2005, Pain on Visual Analogue Scale and evaluation of keratinized gingiva width using customised acrylic stents and UNC 15 probe. The outcomes were assessed at baseline, after 1week and 4 weeks post-operatively. (Figure 1 F&G, Figure 2E&F)
Sample size
Sample size was determined using the estimates of mean and standard deviation values from literature using the formula:
N = 2 (Zα+ Zβ)2 [s]2
d2
where Zα is the z variate of alpha error i.e. a constant with value 1.96, Zβ is the z variate of beta error i.e. a constant with value 0.84.
Approximate estimates:
80% power.
Type I error to be 5%.
Type II error to be 20%.
True difference of at least 1.2 units between the groups.
Pooled standard deviation of 1.4.
Approximately 21 sites per group should complete the trial at the endpoint follow up.
Sampling Technique: Convenience sampling.
Randomisation
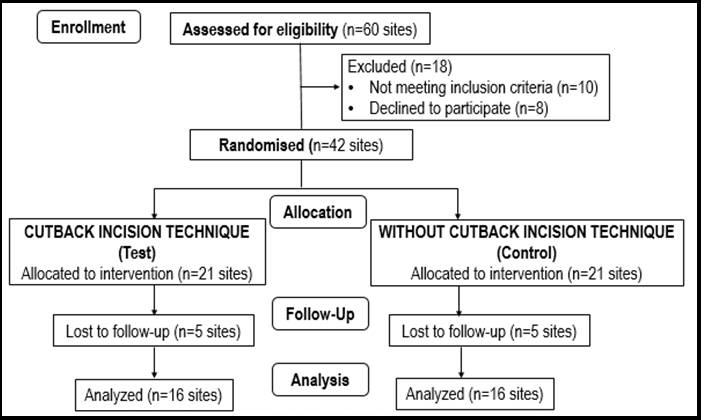
Randomisation was performed and sites were equally divided into two groups: (Figure 3)
Group 1 – Test group and Group 2 – Control group.
Statistical methods
All data were entered into a computer by giving coding system, proofed for entry errors.
Data obtained was compiled on a MS Office Excel Sheet (v 2019, Microsoft Redmond Campus, Redmond, Washington, United States).
Data was subjected to statistical analysis using Statistical package for social sciences (SPSS v 26.0, IBM).
Descriptive statistics like Mean & SD for numerical data has been depicted.
Normality of numerical data was checked using Shapiro-Wilk test & was found that the data did not follow a normal curve; hence non-parametric tests have been used for comparisons.
Inter group comparison (2 groups) was done using Mann Whitney U test.
Intra group comparison was done using Friedman’s (for >2 observations) followed by pair wise comparison using Wilcoxon Signed rank test.
For all the statistical tests, p<0.05 was considered to be statistically significant, keeping α error at 5% and β error at 20%, thus giving a power to the study as 80%.
Results
Participant flow, Recruitment and Baseline Data
In this prospective randomised controlled trial, a total of 42 surgical site augmentation procedures with alloplast + allograft bone substitute were performed: 21 sites with cut back incision technique; and 21 sites with a flapless procedure without cut back incision technique. In both the groups 5 sites were lost to follow-up as the patient did not report for successive follow ups and total of 16 sites per group were assessed for the outcomes. A detailed description of the same is depicted in the CONSORT flow diagram (Fig.3). Data related to the different outcome variables for the intra and inter group comparison was described with respective statistical significance and is reported in tables and graphs respectively.
Outcome and Estimation
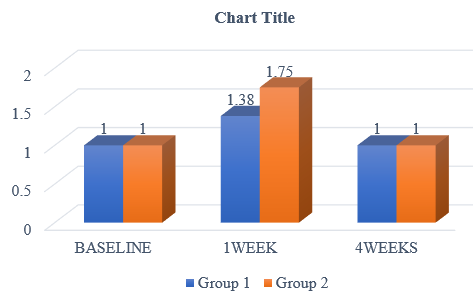
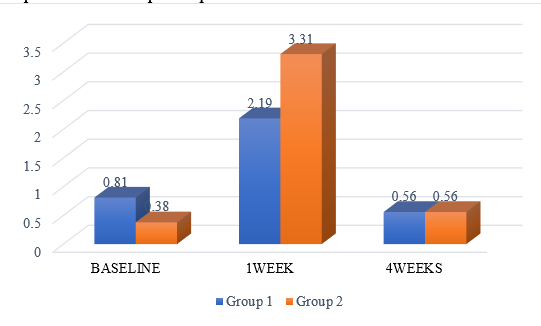
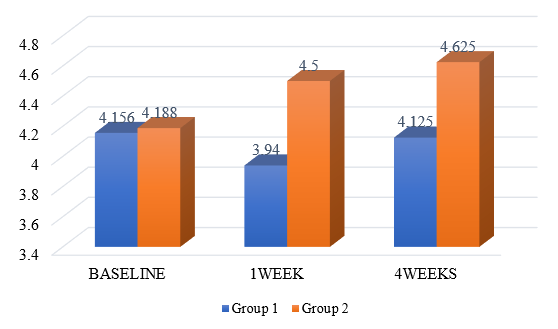
Table 1, Table 2 and Table 3 shows the Intra group comparison in Group 1 of each of the procedures with related results of dependent variables.
Table 4, Table 5 and Table 6 shows the Intra group comparison in Group 2 of each of the procedures with related results of dependent variables.
Table 7 summarises the significant inter group comparisons between the outcome variables related to Group 1 and Group 2 which shows that there was a statistically highly significant difference seen for the values between the groups (p<0.01) for Pain on VAS Scale and KGW 1week with higher values in group 2.
Similar graphical representation of the inter group comparison has been shown in Graphs 1, 2 and 3.
Discussion
Interpretation
Post extraction alveolar ridge resorption and alterations in the soft tissue contour is an inevitable consequence with maximum tissue changes observed during the first month. The extraction site can heal very well without intervention, but if augmentation of the socket with bone is performed, primary closure of the socket is necessary to prevent migration of the bone particles. The relevant literature is rich with several methods, several procedures, different exogenous materials, and soft tissue grafts, free or pedicled, to obtain primary closure of the extraction sockets after bone augmentation.8, 9, 10, 11, 12, 13, 14, 15
This study compares with and without cut back incision technique to obtain and maintain primary closure in extraction sites augmented with particulate bone substitute in attempts to preserve the socket. This technique offers several advantages over the different methods and materials used to achieve primary soft tissue closure of grafted extraction sites.
The cut back incisions promote the coverage of the socket open wound and eliminates the need of additional surgical procedures for harvesting the grafts which may increase post- operative pain, discomfort, haemorrhage or infection.10, 13, 16
The cutback incision technique can also exclude the need for non-autogenous covering materials such as; barrier membranes, mucografts, acellular dermal matrix (alloderm), etc., and so reducing the treatment costs and side effects like infections due to foreign body reaction. The cutbacks are widely used as one of the procedures to lengthen and “advance” the flap into the primary defect, reducing tension at the flap’s tip while eliminating tissue redundancy at the flap’s base. Additional advantages of the back cuts in those medicine areas are; improvement of the flap mobilization, minimizing of the scar length and shifting tensions away from the direction of primary defect closure.17, 18
The cutbacks, when they used for the primary closure of the bone- augmented socket may give the same advantages. They increase the mobilization and the sliding of the flap over the open socket wound, lengthen the flap, and enhance the tension free primary closure over the bone. At the releasing cuts of the flap, the suturing is made also as primary tension free and in this way the blood supply is improved to the flap base and edges. This reduces the infections during the healing period and the scars creation and length thereafter.19
Among the various regeneration techniques, the one proposed in this paper was the filling of the post-extractive alveolus with bone particulate. Two different techniques were consequently adopted: either raising a full flap with cut back incision technique and complete coverage of the socket, or a flapless procedure leaving the socket exposed.
However, one factor which may play a significant role is the type of surgical procedure performed: flap or flapless tooth extraction. Fickl et al. observed that, on a canine model, Open Flap Treatment group had a less bone loss compared with the Close Flap Treatment.20 Conversely, Araujo and Lindhe21 reported that raising a flap during extraction may had an effect on the short-term only. However, the difference between the two techniques was insignificant after 6 months.
In this paper, when the two surgical procedures were compared, some statistical differences were registered. The cutback incision technique encountered significantly more primary closure (p 0.002) and lower pain on VAS (p 0.00) than the control group. Moreover, the analysis of other outcome variable: changes in keratinised gingival width showed no significant difference between test and control group.
On intergroup comparison it shows a statistical higher difference on Pain on VAS (p 0.006) and KGW (p 0.039) at 1 week. Primary healing did not show any statistically significant (p 0.108) at 1week results. However, on further evaluation the difference between the two techniques was insignificant at baseline and at long term follow-up of 4 weeks.
Merits
The present article demonstrates that the primary closure of the bone augmented sockets was obtained using the cut back incision technique with minimal pain and minimal post-operative morbidities.
Also, it minimizes the requirement of using a membrane on the grafted sites.
Dental implants were planned to be inserted in a second stage with adequate bone volume and quality at the recipient sites.
Limitations
Some of the limitations of this study were that no data related to soft tissue biotype was acquired, so it was not possible to assume that different biotypes may result in different dimensional changes.
Also, comparison of different surgical modalities will confirm the effectiveness of different extraction socket preservation protocols.
Further studies and analysis of other variables, such as defect size, and remaining walls condition are essential to confirm the current findings.
Conclusion
Within the limitations of this study, the present findings confirm that preservation of the ridge after tooth extraction is achieved by comparing two surgical techniques. However, the use of cutback incision technique enhances primary closure and the socket seal of the extraction site with minimal pain, morbidity and low cost. Nevertheless, further studies with large sample size and longer follow up duration are required to validate the evidence.