Introduction
Esthetic dentistry is emerging as one of the most progressive and challenging branches of dentistry. The focus of dentistry in the present times is not only the prevention and treatment of diseases but on meeting the demands for better esthetics. Facial beauty and attractiveness has been linked to social perception, where people with a more attractive face are perceived to have higher athletic, social, and leadership skills. The two main components of facial beauty are the face and the dental composition.
The art and science of soft tissues esthetics is an ever evolving field of medicine and dentistry especially periodontology, evidenced by continual development of new surgical and non surgical treatment modalities.1 Nonsurgical rejuvenation procedure such as botulinum toxin (BTX) and dermal filler injections are now the most common aesthetic treatments performed wordwide. According to statistics published by American Society for Aesthetic Plastic Surgery, there was 200% increase in the rate of botox and dermal filler injection techniques since 1997.
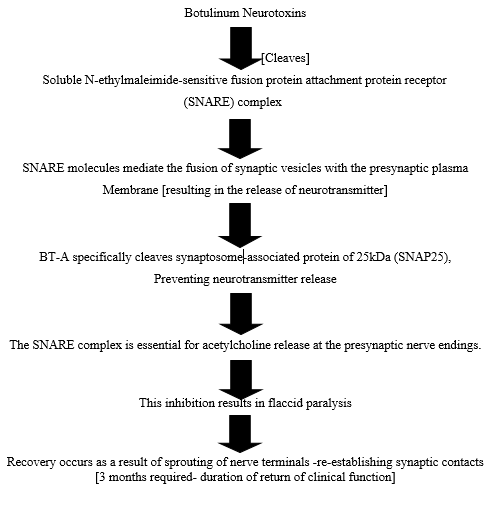
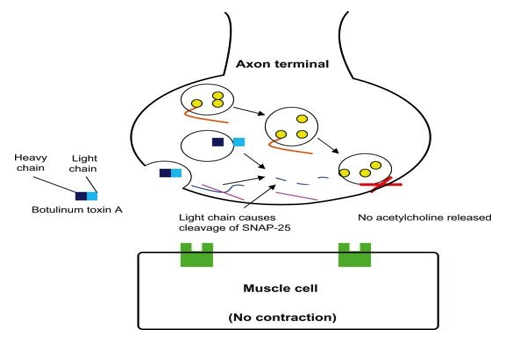
Botulinum toxin (BT) is a neurotoxin produced by anaerobic bacteria clostridium botulinum. It is highly toxic neurotoxin which causes a serious disease called botulism characterised by paralysis of the musculature in the body leading to death which was first noticed by Emile Van Ermengem in 1897.2 BT is a high-molecular weight protein complex made of 3 different proteins: First, a 150-KDa toxin, second, a non-toxin hemagglutinin protein, third, a non-toxin non-hemagglutinin protein. 3 Botulinum toxin can be differentiated serologically into eight kinds of toxins named from A to G (A, B, C1, C2, D, E, F, and G). 4, 5 Neurotoxin strains A and B are antigenically different, but have similar functions and are commercially available for medical treatments. 6, 7
History
The German physician and poet Justinus Kerner 8 first developed the idea of a possible therapeutic use of botulinum toxin, which he called “sausage poison”. In 1870, Muller 9 (another German physician) coined the name botulism. In 1949, Dr. Burgen's group discovered that botulinum toxin blocks neuromuscular transmission.In December 1989, (BOTOX®) was approved by the United States Food and Drug Administration (US FDA) for the treatment of strabismus, blepharospasm, and hemifacial spasm in patients aged younger than 12 years.10 On December 21, 2000, Botox received US FDA approval for treatment of cervical dystonia.11 On April 15, 2002, the US FDA announced the approval of BOTOX® Cosmetic to temporarily improve the appearance of moderate-to-severe frown lines between the eyebrows (glabellar lines).On September 11, 2013, the US FDA approved BOTOX® for the temporary improvement in the appearance of moderate to severe lateral canthal lines, known as crow’s feet. This is the only FDA-approved drug treatment option for lateral canthal lines.
Application of botox
General appliction
Overactive bladder
Upper limb spasticity in adult patients
Prophylaxis of headaches in adult patients with chronic migraine
Cervical dystonia in adult patients (severe neck muscle spasm)
Blepharospasm (spasm of the eyelids)
Strabismus (Squint)
Rhinitis
Hyperhidrosis
Foot dystonia
Tremor
Spasticity
Induce ptosis/Reduce lid retraction
Laryngeal dystonia
Benign prostatic hyperplasia
Stammering/stuttering
Maxillofacial applications
Cosmetic applications
a. Facial Wrinkles: The first signs of aging are often wrinkles around eyes, forehead, cheeks, and lips.
Wrinkles are a normal feature of the human face but are unaesthetic. Botox is an effective way to reduce the appearance of wrinkles
b. Drooping of corners of mouth: Hyperactivity of depressor anguli oris can lead to drooping of the corner of the mouth. Injection of Botox has shown to have positive results in such cases. 12
c. In post-radiosurgical neck contracture: In post-radiosurgical neck contracture, botox injection is a simple and easy procedure able to improve neck motion and reduce neck pain in head-and-neck cancer patients.
Therapeutic applications (Non cosmetic application
The diverse group of TMDs those are likely to be benefited by injection of Botox includes the following: 13
Bruxism and clenching
Oromandibular Dystonia
Hemifacial Spasm
Myofascial Pain
Masseter and temporalis hypertrophy
Sialorrhea and salivary disorders
Facial nerve palsy
Facial pain trigeminal neuraligia
Oral and maxillofacial trauma
Cancer and palliative care
Denture Wearers
Adjunct to orthodontic treatment and to prevent relapse
An adjuvant for wound healing after oral and maxillofacial surgery
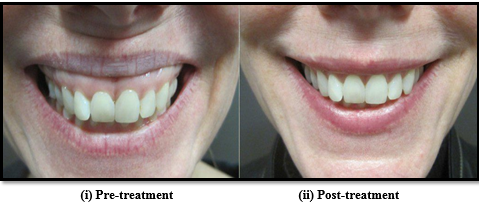
Gummy smile
The smile is considered the most pleasant and complex of all the facial expressions. 14 It has been said that “a smile is one of the most effective means by which people convey their emotions”. 15 A person’s smile depends on three main components: teeth, gums, and lips. Many have studied the components of an attractive smile; most studies concluded that the perfect amount of maxillary gingival tissue shown during smiling is 3 mm. 15 Gummy smile, or excessive gingival display in the maxillary arch on smiling, is known as the difference between the lower margin of the upper lip and the superior margin of the incisors and is considered one of the most embarrassing and self-conscious cosmetic aspects in humans. 16 Gummy smile should be first classified either according to the area of the maxilla shown, i.e., anterior, posterior, mixed, or asymmetric, or via the Goldstein classification as low, medium, or high based on the amount of exposure. 15 This classification is important to identify the involved muscle and to modify the injection technique of Botox type I. 14 The effect of Botox will appear after 2 weeks and persists between 4 and 6 months depending on the muscle thickness and anatomy. 17
Etiological factors involved in the formation of gummy smile can be, Skeletal (vertical maxillary Skeletal (vertical maxillary excess), Gingival (passive eruption) or Muscular (hyper functional upper lip) and treatment options range from Le fort I osteotomy, crown lengthening, intrusion, myectomy to muscle resection etc. Botox is indicated when the gummy smile is due to hyper functional upper lip elevator muscles (muscular capacity to raise the upper lip is higher than average)
Procedure for injection
For correction of gummy smile, Botox is injected into the hyperactive elevator muscles of lip blocking excessive contractions and thus prevent the lip from being pulled too far up while smiling. It will be important for the patient to avoid taking aspirin or related products, such as ibuprofen (e.g., Advil) or naproxen if possible after the procedure to keep bruising to a minimum. Prior to injection, reconstitute vacuum-dried BOTOX, with sterile normal saline without a preservative; 0.9% Sodium Chloride Injection is the only recommended diluents. Draw up the proper amount of diluents in the appropriate size syringe, and slowly inject the diluents into the vial. BOTOX should be administered within four hours after reconstitution.During this time period, reconstituted BOTOX should be stored in a refrigerator (2° to 8°C). Reconstituted BOTOX should be clear, colorless and free of particulate matter.
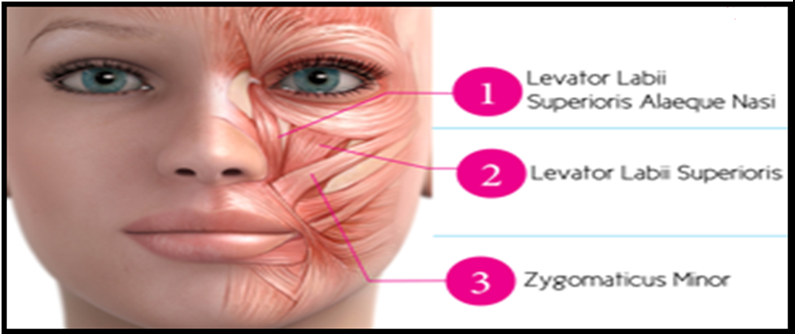
Mark polo 18 has advocated the ideal dosage might be 2.5 U/0.1ml per side at the LLS & LLSAN, 2.5 U/0.1ml per side at the LLS/ZM sites, and 1.25 U/0.1ml per side at the OO sites. Hwang et al, 14 Yonsei University College of Dentistry, Seoul, Korea have proposed a injection point for botulinum toxin-A, and named it as YONSEI POINT and they recommend a dose of 3U at each Yonsei point.Yonsei point is located at the centre of the triangle formed by:
Levator labii superioris [LLS],
Levator labii superioris alaeque nasi [LLSAN],
Zygomaticus minor [Zmi]
After the injection, the patient was instructed to avoid lying down , exercising, or massaging the injection site lying down for 4 hours. 14 Two weeks later, post injection photos were taken at the same position of the pre-injection. Effect of botox is seen within 5-10 days and last about 6 months, with a range of 4 to 8 months, at which time the patient can return to repeat the process. It is important not to give injections prematurely (before the effects of the treatment have worn off), as this can result in a buildup of antibodies to botox that would dilute the effect of further treatments.
Dental Implants
Excessive functional forces, especially in patients with parafunctional habits can hamper the process of osseointegration. Thus, the overloading of implant results in its failure. Forces from hyperactive masticatory muscles can also prevent or impede fracture callus formation after maxillofacial fracture fixation. Hence in both conditions muscular relaxation can be achieved with Botox injections into the masticatory muscles allowing a more stable environment for implant integration and fracture healing.19 Etiological factors involved in the formation of gummy smile can be, Skeletal (vertical maxillary excess), Gingival (passive eruption) or Muscular (hyper functional upper lip) and treatment options range from Lefort I osteotomy, crown lengthening, intrusion, myectomy to muscle resection etc.
Contraindication
The following conditions are contraindicated with this drug.
Allergy to botulinum toxin
Lou Gehrig's Disease
Disorder of the Peripheral Nerves that Cause Movement
Myasthenia Gravis
Progressive Muscle Weakness with Carcinoma
Condition Where One Object Appears as Two or More Object
Double Vision
Blurred Vision
Drooping of the upper eyelid
Infection of Lung from Inhaling Stomach Contents
Decreased Lung Function
Voice disorder
Hoarseness
Dysarthria
Trouble Breathing
Difficulty Swallowing
Problems with Bladder Control
Post operative care for patients
Treated area should not be manipulated for 3 hours following treatment.
Any facial/laser treatments or microdermabrasion after Botox injections for at least 10 days should not be conducted.
Some providers believe that smiling and frowning right after botox treatments helps the Botox find its way to the muscle into which it was injected after treated.
Patients should be instructed not to lie down for 4 hours after your Botox treatment. This will prevent tracking into the orbit of your eye and causing drooping eyelid.
It can take approximately 4 to 7 days for results to be seen. If the desired result is not seen after 2 weeks of your treatment additional Botox may be required.