Introduction
The pandemic of coronavirus COVID-19 that started in January 2020 is gradually engulfing the world population. According to the world meters of corona virus, to-date 17th March 2020, 183,325 confirmed cases of corona virus, with a death toll of 7,177 deaths.1 World health organization has internationally declared it as public health emergency.2 This virus was transmitted from a single animal to human source and later on spread through human to human transmission.3 Routes of transmission of this virus are via respiratory droplets, direct or indirect contact (fomites) transmission,4 and possible orofecal transmission, due to presence of virus within stools of infected individuals.5
An infected person has the potential to transmit this infection during asymptomatic phase of incubation period6 Hubei province, China. Affected patients were geographically linked with a local wet market as a potential source. No data on person-to-person or nosocomial transmission have been published to date. Methods: In this study, we report the epidemiological, clinical, laboratory, radiological, and microbiological findings of five patients in a family cluster who presented with unexplained pneumonia after returning to Shenzhen, Guangdong province, China, after a visit to Wuhan, and an additional family member who did not travel to Wuhan. Phylogenetic analysis of genetic sequences from these patients was done. Findings: From Jan 10, 2020, we enrolled a family of six patients who travelled to Wuhan from Shenzhen between Dec 29, 2019 and Jan 4, 2020. Of six family members who travelled to Wuhan, five were identified as infected with the novel corona virus. Additionally, one family member, who did not travel to Wuhan, became infected with the virus after several days of contact with four of the family members. None of the family members had contacts with Wuhan markets or animals, although two had visited a Wuhan hospital. Five family members (aged 36–66 years, active state of disease and even during the recovery phase.7 This prospective further aggravates the spread of disease. As dentists work in close proximity of oral cavity, are not only at highest risk of getting infected 8 but can be a possible source of spread of infection to other non- infected individuals. Absence of sufficient evidence of definitive guidelines on the subject can further interfere with the effective control of spread of this infection.
The School and Hospital of Wuhan University provided an overview of their practices during the coronavirus outbreak.9 Record of patient’s as well as practitioner’s contact with infected individuals at home or at work, patient’s contact details, travel history and history of attending a large gathering in recent past, help to identify susceptible individuals. Temperature record, maintenance of hand hygiene, prompt surface disinfection, and use of face mask with protective eye shields are prerequisites to prevent cross infection. However, as for other type A infections, special measures are recommended to minimize the spread of disease.9 These include record implementation of four handed dentistry for emergency procedures only, preoperative mouthwash rinses, and use of high vacuum evacuation with saliva ejectors.10
In, India, the total number of registered general dental practitioners Lucknow & Barabanki district Uttar Pradesh, India is more than 20,000.11 This increasing number can be a huge risk for all health professionals12 as well as general public. It is a dire need of the day to spread the information about prevention and mandatory dental practices, relevant to COVID-19 across country, to curtail the possible effects of corona- virus explosion. The information can be communicated through general mainstream media as well as through specifically directed professional contacts. The aim of this study was to evaluate the awareness of cross infection control measures during stage I of pandemic of COVID-19 within dental practices of Pakistan.
The rationale of this study was to identify the deficient areas and misconceptions in the knowledge of dental practitioners, about precautionary measures against COVID-19, so that timely guidelines can be given to address those deficiencies and encourage the minimization of infection transmission as much as possible.
Materials and Methods
A cross sectional survey of knowledge of cross infection control measures specific to corona virus was performed on amongst general dental practitioners. During the initial stages of spread of corona virus in India,13 from 15th March 2020 – 17th March 2020.
The study conforms to STROBE guidelines for human observational studies. The survey form comprising of ten questions regarding cross infection control for COVID-19 was generated, using the guidelines of The School and Hospital of Wuhan University.9 the content and validity of questionnaire were assessed by 2 experts.
The study population included all those general dental practitioners who are presently in service at various clinics and dental hospitals across Lucknow & Barabanki district Uttar Pradesh, India. Survey form was not sent to those who are not actively involved in clinical dentistry. A non-probability convenience sample method was used. By using 95% confidence interval, calculated sample size was 149. Survey was sent to 200 dentists, to avoid non respondents. 148 participants responded. Non respondents were excluded from data analysis to eliminate error.
Consent of each participant was taken by their acceptance to fill out the form. The participants were asked to fill out questions regarding personal protection equipment, means to trace the source of infection during history and clinical examination, precautionary measures to preoperatively reduce the number of microbes, types of procedures to be performed during the COVID-19 outbreak, means of irrigation and saliva ejection mechanism, recommended radiographic techniques and protocol for surface disinfection.(Table 1) All questions had multiple choice answers from participants had to elect one best option only. All forms were submitted electronically to expedite the information transmission and prevention of human to human contact.
The data was collected within two days to analyze the awareness levels at the start of outbreak. The time period for data collection was kept short to minimize the possibility of false positive results of better awareness levels. The confidentiality of all the subjects regarding their personal and professional information was assured. The data collected was analyzed on SPSS version 23.0. Descriptive analysis was done. Percentages of each answer were utilized to assess the awareness level of general dental practitioners. 66% or more correct answers out of 10 signified adequate awareness amongst participants.14
Results
148 participants responded to the survey. Following the 7 or more (66%) correct answers criteria, there are 135 out of 148 participants (91%) who have satisfactory level of awareness regarding the protective measures. The result is displayed in the following pie chart. (Figure 1)
By considering the total scores for each participant, following descriptive measures are calculated. Mean score was 8.36, Mode (most frequent score) was 9, minimum score was 4 while the Maximum score was10. The percentages of highly recommended protection control measures are given in Figure 2. By considering the total scores for each participant, following descriptive measures are calculated.
Discussion
This study was conducted to evaluate awareness of cross infection control measures amongst general dental practitioners of Lucknow & Barabanki district Uttar Pradesh, India. The results of study showed a general positive trend towards better awareness (91% satisfactory level). Utilization of complete kit of personal protective measures including surgical gowns, face mask (N-95 or FFP2 masks), 14 face shields or protective eye wear reduces the possibility of contact transmission through oral, nasal and eye routes. In addition, as the virus can stay virulent from few hours to days on different surfaces, so it is a better practice to provide complete coverage to skin, mucosa as well as personal garments. The protective equipment once used must be disposed off to prevent further contamination to other surfaces.
In addition to medical history, contact details of a dental patient can be helpful in locating a possible source of infection, especially in case of an aftermath of an unnoticed exposure to dental personnel. However, individual role of this detail was not considerable for majority participants of this study. Notifications to concerned authorities about such portals of infection can not only block their chain of transmission but also help in provision of timely management to the infected person.
Record of patient’s travel history takes precedence over medical history for apt diagnosis of this condition. Epidemiological information of patients within past 14 days,9 even before the onset of symptoms, would help in locating a possible carrier as well as the cause for an existing clinical presentation. In this study, majority participants preferred both options; however it must be stressed to consider the purpose of each one of them.9
Utilization of temperature sensors15 for recording temperature of every staff and patient is recommended as a regular procedure. Persons with fever must be referred to a concerned hospital for thorough evaluation. In the present study, 31.08% considered both records as important; however, this should be discouraged as while recording pulse, physical contact with an affected person can compromise the infection control measures against for the operator.
Use of preoperative mouth rinse with chlorhexidine containing mouth washes can reduce the number of microbes in oral cavity.10 This can reduce the potential risk of cross contamination with operator from an infected patient. However, use of a preoperative tap water rinse is not backed scientifically over multiple forums. Water rinse or intake may not be beneficial for washing away of virus, as it can enter through nose and eyes too, where gastric juices will not be able to digest it. However, general hydration is beneficial as in other common viral infections.16
Figure 1
Cross infection control awareness levels ofLucknow & Barabanki district Uttar Pradesh, India dentist for COVID-19.
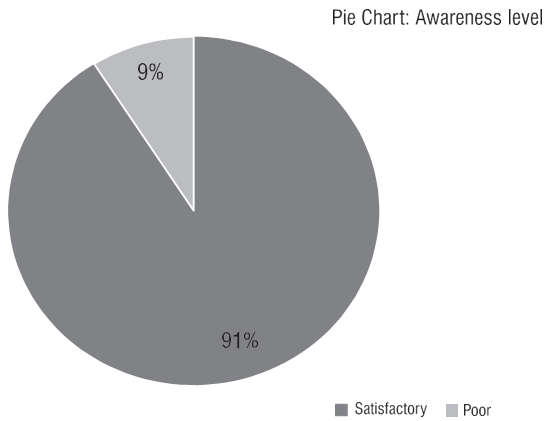
Figure 2
Percentages of highly recommended infection control measures for protection against transmission of COVID-19
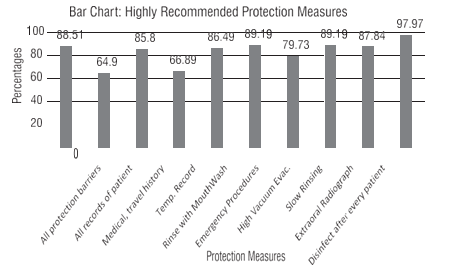
Table 1
Questionnaire used for assessing cross infection control awareness of Pakistani dentists for covid-19 pandemic, with frequencies and percentages.
Majority of the participants were of opinion to perform emergency procedures only. Acceptance of this limitation can improve the cross infection control measures. However, in each specialty the definition of emergency procedure is still controversial. A dental emergency during COVID-19 pandemic is considered only when no other nonintervention treatment is helpful to alleviate the complaint. 17 All other procedures must not be practiced. This approach will maintain the quarantines amongst the effected and unaffected onces. Use of high volume saliva ejection reduces the aerosol production which can help in maintenance of cross infection control. 10 Most of the participants responded in favor of acquiring this system. It is indeed important to highlight again that only emergency procedures would be performed, for which high vacuum ejection would be required. Air stream projecting with water stream from a triple syringe can propel patient’s fluids to spill over adjacent surfaces, thus breaching protection protocol. It is therefore advised to use slow rinsing of wounds to avoid scattering. This can be done by an assistant with a hand held disposable syringe, in a four handed technique. 18
Table 2
Recommended guidelines to prevent coronavirus transmission in a den- tal setting.19
Table 0
Intra oral radiographs are indicated for endodontics procedures, however placement of an intra oral film allows greater exposure of surfaces but it may also initiate increased salivary secretions20 and gag reflex, with subsequent coughing, or vomits. This can aggravate the infection transmission. To avoid this, extra oral radiographs i.e. panoramic view or CBCT can be utilized as CBCT provides three dimensional analyses from either labial or palatal sides.21
COVID-19 virus has the potential to survive on metal and plastic surfaces for more than 48 hours.22 Prompt disinfection of dental unit surfaces after check- up/emergency procedures of every patient may reduce the likely hood of infection transmission. Earlier, 0.5% hydrogen peroxide, 62–71% ethanol or 0.1% sodium hypochlorite for 1 min were considered more effective surface disinfectants for corona virus but it lacks recent evidence.23
In light of the evidence(9) of COVID-19 pandemic, following guideline 19 might prove beneficial to general dental practitioners during such situation. (Table 2)
This assessment tool (Table 1), can be utilized in areas where COVID-19 outbreak is at initial stages, in order to evaluate the level of awareness of dental professionals. This will help in overcoming the barriers to the spread of pertinent information in this regard.
Conclusion
COVID-19 is moving towards a worldwide exponential growth including India. Earlier awareness of Covid-2 specific protection measures to health professionals may reduce the number of new diseased cases. Aggressive maintenance of social distancing generally and strict adherence to corona specific cross infection control protocol in a dental setting might help in effective control of this potentially deadly disease.
