- Visibility 79 Views
- Downloads 18 Downloads
- Permissions
- DOI 10.18231/j.ijpi.2020.031
-
CrossMark
- Citation
Epigenetics and pathogensis: A newflanged review
- Author Details:
-
Avineet Kaur *
-
Harnoor Singh Sandhu
-
Kanwar Shabaz
-
Surinder Sachdeva
-
Raman Chopra
-
Shailja Chatterjee
Abstract
Genetics and epigenetics is the process of gene expression or suppression through polymorphism, demethylation, and deacetylation. Although Periodontal diseases are bacterial infections predominantly gram negative anaerobic bacteria that colonize the sub gingivaly in return triggering an inflammatory response which affect the periodontium; whereas periodontitis is a periodontal disease which destroys the tissue and bone that surrounds the tooth. In adults periodontitis is at helm of tooth loss. Pathogenic microrgansims are considered as the primary aetiological factor, but the disease progression is also influenced by Genotype and Phenotype of various individuals. Phenotypic factors such as race, diabetes, gender, education, smoking etc. have sweeping effects on the epigenetic changes and impel susceptibility to disease. Epigenetic modifications expression occur in response to environmental changes.
Introduction
Epigenetics is a field that deals with study of epigenome. Word “Epi” means outside the “genome”.[1]
Waddington H. C. coined the word Epigentics[2] describing it as a“causal mechanisms” by which genes give rise to the phenotype. Epigenetics is described as changes in gene expression not encoded in DNA sequence, which may take the form of chemical modifications of DNA and concomitant proteins, which are responsible for remodeling of the chromatin and activation or inactivation of a particular gene.[3], [4] Periodontitis is a disease in which chronic inflammation of gingival tissues takes place in response to bacteria. In definite individuals, immune response leads to tissue destruction and bone loss alongwith connective tissue. Periodontitis is very common diseases in humans undoubtedly including 10% of adult population.[5] According to survey it has been observed that periodontitis is sixth-most prevalent condition worldwide.[6] Periodontitis is a disease involving an interplay of various factors with its absolute mechanism remaining unclear, but a contributing factor for inflammation and infection is the presence of multiple disease inducing microorganisms of the likes of Tannerella forsythia, Aggregatibacter actinomycetemcomitans and Porphyromonasgingivalis, which in turn triggers host immune response[7] In Cold Spring Harbor Meeting which was held in 2008, described epigenetics as “stable heritable phenotype which results from alterations in chromosome without changes in DNA pattern”.[8] In Greek language prefix ‘epi-’ in epigenetic means in addition to genetics. Epigenetics acts as a cross linkage between genetics , environmental and lifestyle factors whose alteration may come up in an individual showing differences in local gene expression leading to inflammation and susceptibility for the disease. Although Epigenetics research is still in nascent stage but it holds promise in positively influencing the causative factors affecting oral health and hygiene. Therefore Epigenetics denotes a strong link between environment and phenotype.[9]
Brief about periodontitis
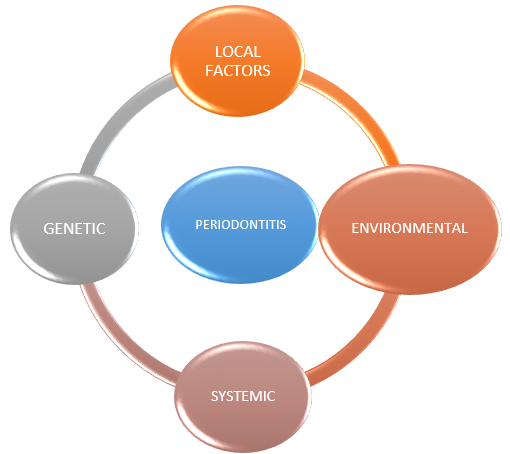
Periodontitis is a complex disease which is characterized by inflammation and destruction of tooth supporting structures. Aetiology behind periodontitis is an interplay of various other factors which include both genetical components, microflora, host immune response and other phenotypic etiologic agents.[10] Gene which is specific possesses different epigenetic patterns depending on the cell type thus resulting as a local and systemic expression of the gene. In 1970s microflora associated with dental plaque was considered to be a sole factor. But further evidence found that bacteria were essential but not singular in producing disease. Host response dictates susceptiblity to diseases.
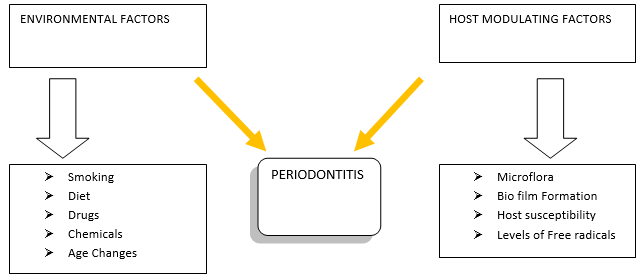
Phenotypic factors might affect gene regulation leading to epigenetic alteration in the genome. It is determined that host microbial interactions and environmental factors are major determinants for the development of periodontal disease. So it specifies the relationship between genotype and phenotype.[11]
Epigenetics and modifications
Epigenetic modification are of three types There are three types seen as DNA methylation, histone modification and RNA-associated silencing (micro-RNA).[11], [12] During replication it was observed that the processes of demethylation, acetylation, methylation, deacetylation and their combinations worked to express or repress genes. Studies conducted back by Griffith and Mahler in 1969 DNA methylation and well characterised epigenetic modification is one of the most broadly studied Dna Methylation and well characterised epigenetic modification may be important in long term memory function.[13] These processes are initiated by environmental influences which regulate cytokines such as IL6 and IL1 responsible for inflammatory tissue response. Thus susceptibility of individual to periodontitis depends on his immune response. Therefore decrease in number of neutrophils also increases the susceptibility of infections.
It was found that the polymorphism in IL 1 is more damaging as it performs to a singularly piquant role in the formulation of inflammatory response. Many Studies suggested that individuals having greater levels of IL1 show a greater preponderence to periodontitis as opposed to those having less level.[14]
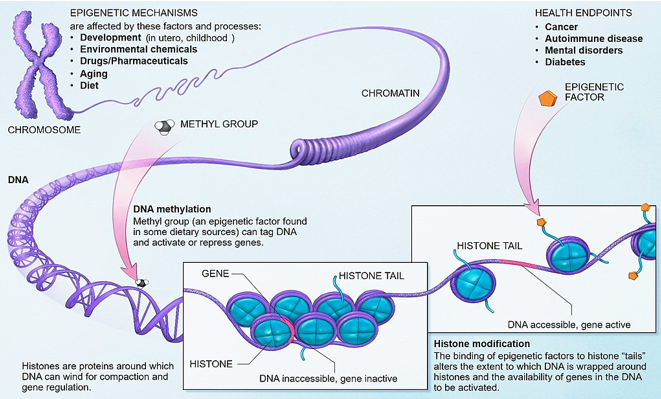
Alteration of histone proteins and DNA methylation
A gene is seen to be the instructional portion of DNA which helps in that signalling biological activity. DNA methylation is a sequence of chemical reactions that can either cause an addition of a particular methyl group attached to a DNA molecule (hypermethylation) or cause a subtraction (demethylation) of a group, a process facilitated by[15] histone proteins. Acetylation creates a loosely compacted DNA complex which allows for gene expression in contrast to deacetylation which leads to densely compacted DNA expression. An intense correlation has been observed of gene expression with histone modification/ DNA methylation.[16] These reaction leads to change in gene expression which leads to change in biological activity while maintaining the DNA sequence as it is. The two most common epigenetic factors are nutrition and aging. Effects on epigenetics can be observed in cases in which there are deficiency of folic acid and deficiencies of selenium, arsenic and polyphenols. These deficiencies can lead to various diseases like neural tube defect and malignancies. A study reported by Wilson on epigenetic factor aging methylation and acetylation process were carried out in mono zygotic twins and very similar results were seen in early life and substantial differences in later life. Various Environmental influences contribute to the progression of periodontitis. Some environmental stressors have been reported to begin before birth though some epigenetic marks are potentially reversible, many epigenetic changes appear to persist throughout the life of the organism several factors which are responsible for epigenetic modification are diabetes, race, gender, BMI etc. One of the important environmental risk factors for progression of periodontitis is smoking. Smoking causes long term hypo and hypermethylation changes in the DNA. A study observed by Haffajee and Socransky found that smokers had more severe form of periodontitis with more attachment loss and deeper pockets compared with non-smokers. [16]
This review here focuses the importance of genetic factors which leads to highlights the interplay mechanism b/w periodontal disease and epigenetic alterations
Epigentics and periodontitis – The Connection
Chronic inflammatory diseases, by nature are tissue specific. Epigenetic changes occur locally at the biofilm-gingival interface surrounding the neck of teeth and epigenetic alterations differ relative to an inflamed periodontital tissue site and non-inflamed sites. [17], [18]
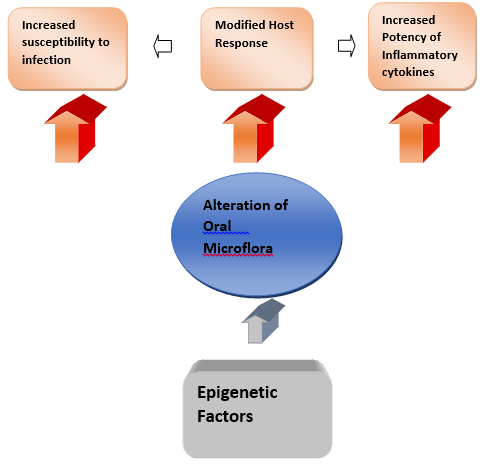
Negative modifications in the epigenome are caused due to infection and host immune response. The epithelium, of the oral cavity functions as the first line of defense that alternates epigenome in these cells leads to subsequently alteration in inflammatory cells, which contribute to a crux of modifications in the signaling pathways and gene expression. Oral microflora cause acetylation and down-regulation of DNMT1, causing activation of PRRs and TLRs leading to induced histone changes in epithelial cells.[19]
TLRs play a crucial role in innate immunity of an individual through their ability to perceive and differentiate between pathogen-associated molecular patterns (PAMPs) and bacterial lipopolysaccharide (LPS). Disturbance in regulation of TLR expression influences the host response leading to increased degree of inflammatory response and susceptibility to periodontitis. Activated TLRs induce histone acetylation and activation of transcription factor Nuclear factor-κb (NFκB). NFκB is a transcription factor that causes differentiation of and induces Matrix metalloproteinases (MMPs) production.[20] Surface receptors influence attachment of cells to ECM, inducing MMPs expression,.[21] Interestingly, healthy individuals and periodontitis patients have variations in genes related to immune response.[22]
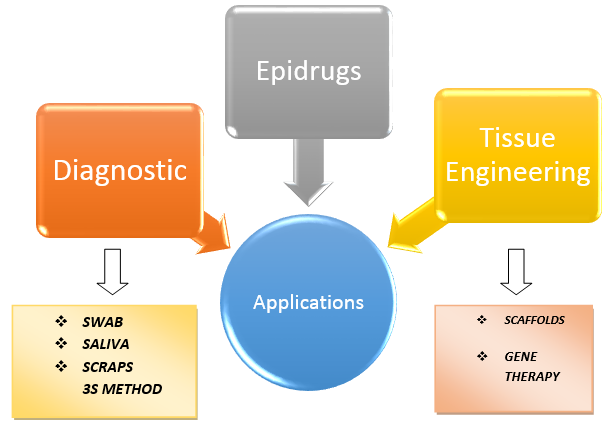
Diagnosis & Epidrugs
Epigenetic pattern can be utilized as a marker to identify a clinical phenotype which can be utilized to determine individuals who are at risk of periodontitis by utilizing buccal swabs, saliva or scraping of the oral mucosa for epigenetic analysis
This approach is profoundly useful in screening and confirmation of patients with oral malignancy.
Epidrugs a term coined by Ivanov and co-workers, is a drug which inhibits or activates disease-associated epigenetic proteins which regulate ameliorating, cure, or prevention of the disease.
Numerous studies utilising epidrugs have been conducted in the field of oncology and nutrition as treatment modalities but there is paucity of research on epidrugs with regard to oral health.
Tissue Engineering
A goal of periodontal tissue engineering/regenerative medicine is to restore all the periodontal components, i.e., the ligament, cementum, bone and surrounding soft tissues. [23] Scaffolding and gene therapy are major tools for tissue regeneration.
Scaffolds with nano engineered topography is a tool to improve outcomes of periodontal tissue engineering. [24] Nanotechnology enhances tissue regeneration and cellular functional capability through the medium of epigenetics while tissue regeneration can be improved by combining scaffold characteristics with delivery of epidrugs, Human gingival fibroblasts (HGFs) act as a source for periodontal tissue regeneration.
Future concepts of epigenetics
Epigenetics is a complex field with DNA reactions linked together regulating gene expression
Epitranscriptome is a new field that have emerged. RNA stability and translation as well as RNA splicing, is affected by epigenetics. Variants of methylation of adenine within RNA have been identified, i.e., N6-methyladenosine (m6A) and the further methylated form N6, 2-O-dimethyladenosine.
Periodontitis is a complex disease with a plethora of cells, cytokines, and signaling pathways involving the activation and regulation of the immune response.
Conclusion
Several key factors which can induce epigenetic alterations, affect the oral health adversely Research has been carried out on the influence of bacteria and inflammation, how diet and smoking influence epigenetic mechanisms needs indepth understanding.
Source of Funding
No financial support was received for the work within this manuscript.
Conflict of Interest
The authors declare they have no conflict of interest.
References
- Lavu V, Venkatesan V, Rao V. RThe epigenetic paradigm in periodontitis pathogenesis. J Indian Soc Periodontol. 2015;19(2):142-9. [Google Scholar]
- . Lena Larsson Current Concepts of Epigenetics and Its Role in Periodontitis. Curr Oral Health Rep. 2017;4(4):286-93. [Google Scholar]
- Waddington CH. The epigenotype. Int J Epidemiol. 2012;41:10-3. [Google Scholar]
- Bird A. DNA methylation patterns and epigenetic memory. Genes Dev. 2002;16(1):6-21. [Google Scholar] [Crossref]
- Eke P, Dye B, Wei L, Thornton-Evans G, Genco R. Prevalence of Periodontitis in Adults in the United States: 2009 and 2010. J Dent Res. 2012;91(10):914-20. [Google Scholar] [Crossref]
- Kassebaum N, Bernabé E, Dahiya M, Bhandari B, Murray C, Marcenes W. Global Burden of Severe Periodontitis in 1990-2010. J Dent Res. 2014;93(11):1045-53. [Google Scholar] [Crossref]
- Ari G, Cherukuri S, Namasivayam A. Epigenetics and Periodontitis: A Contemporary Review. J Clin Diagn Res. 2016;10(11):7-9. [Google Scholar]
- Berger SL, Kouzarides T, Shiekhattar R, Shilatifard A. An operational definition of epigenetics. Genes Dev. 2009;23(7):781-3. [Google Scholar] [Crossref]
- Abraham S, Saseendran G, RA. Epigenetics - A Window Towards Personalized Periodontal Therapy. IOSR J Dent Med Sci. 2017;16(6):33-7. [Google Scholar] [Crossref]
- Lindroth A, Park Y. Epigenetic biomarkers: a step forward for understanding periodontitis. J Periodontal Implant Sci. 2013;43(3):111-20. [Google Scholar] [Crossref]
- Bayarsaihan D. Epigenetic Mechanisms in Inflammation. J Dent Res. 2011;90(1):9-17. [Google Scholar] [Crossref]
- Egger G, Liang G, Aparicio A, Jones P. Epigenetics in human disease and prospects for epigenetic therapy. Nat. 2004;429(6990):457-63. [Google Scholar] [Crossref]
- Holiday R. Epigenetics: A historical overview. Epigenetics. 2006;1:76-80. [Google Scholar]
- Tarannum F, Faizuddin M. Effect of gene polymorphisms on periodontal diseases. Indian J Human Genet. 2012;18(1):9-19. [Google Scholar] [Crossref]
- Yehuda R, Bierer L. The relevance of epigenetics to PTSD: Implications for the DSM-V. J Trauma Stress. 2009;22(5):427-34. [Google Scholar] [Crossref]
- Wilson AG. Epigenetic regulation of gene expression in the inflammatory response and relevance to common disease. J Periodontol. 2008;79:1514-9. [Google Scholar]
- Larsson L, Castilho R, Giannobile W. Epigenetics and Its Role in Periodontal Diseases: A State-of-the-Art Review. J Periodontol. 2015;86(4):556-68. [Google Scholar] [Crossref]
- Barros S, Offenbacher S. Modifiable risk factors in periodontal disease. Periodontol. 2014;64(1):95-110. [Google Scholar] [Crossref]
- Martins M, Jiao Y, Larsson L, Almeida L, Garaicoa-Pazmino C, Le J. Epigenetic Modifications of Histones in Periodontal Disease. J Dent Res. 2016;95(2):215-22. [Google Scholar] [Crossref]
- . Abu-Amer Y. NF-kappaB signaling and bone resorption. Osteoporosis Int. 2013;24:2377-86. [Google Scholar]
- Takai R, Uehara O, Harada F, Utsunomiya M, Chujo T, Yoshida K. DNA hypermethylation of extracellular matrix-related genes in human periodontal fibroblasts induced by stimulation for a prolonged period with lipopolysaccharide derived fromPorphyromonas gingivalis. J Periodontal Res. 2016;51(4):508-17. [Google Scholar] [Crossref]
- Souza AD, Planello A, Marques M, Carvalho DD, Line SP. High-throughput DNA analysis shows the importance of methylation in the control of immune inflammatory gene transcription in chronic periodontitis. Clin Epigenet. 2014;6(1). [Google Scholar] [Crossref]
- Larsson L, Decker A, Nibali L, Pilipchuk S, Berglundh T, Giannobile W. Regenerative Medicine for Periodontal and Peri-implant Diseases. J Dent Res. 2016;95(3):255-66. [Google Scholar] [Crossref]
- Du M, Duan X, Yang P. Induced Pluripotent Stem Cells and Periodontal Regeneration. Curr Oral Health Rep. 2015;2(4):257-65. [Google Scholar] [Crossref]
- Abstract
- Introduction
- Brief about periodontitis
- Epigenetics and modifications
- Alteration of histone proteins and DNA methylation
- Epigentics and periodontitis – The Connection
- Diagnosis & Epidrugs
- Tissue Engineering
- Future concepts of epigenetics
- Conclusion
- Source of Funding
- Conflict of Interest
- References
How to Cite This Article
Vancouver
Kaur A, Sandhu HS, Shabaz K, Sachdeva S, Chopra R, Chatterjee S. Epigenetics and pathogensis: A newflanged review [Internet]. IP Int J Periodontol Implantol. 2020 [cited 2025 Sep 14];5(4):134-138. Available from: https://doi.org/10.18231/j.ijpi.2020.031
APA
Kaur, A., Sandhu, H. S., Shabaz, K., Sachdeva, S., Chopra, R., Chatterjee, S. (2020). Epigenetics and pathogensis: A newflanged review. IP Int J Periodontol Implantol, 5(4), 134-138. https://doi.org/10.18231/j.ijpi.2020.031
MLA
Kaur, Avineet, Sandhu, Harnoor Singh, Shabaz, Kanwar, Sachdeva, Surinder, Chopra, Raman, Chatterjee, Shailja. "Epigenetics and pathogensis: A newflanged review." IP Int J Periodontol Implantol, vol. 5, no. 4, 2020, pp. 134-138. https://doi.org/10.18231/j.ijpi.2020.031
Chicago
Kaur, A., Sandhu, H. S., Shabaz, K., Sachdeva, S., Chopra, R., Chatterjee, S.. "Epigenetics and pathogensis: A newflanged review." IP Int J Periodontol Implantol 5, no. 4 (2020): 134-138. https://doi.org/10.18231/j.ijpi.2020.031
