Introduction
Frenectomy or frenulectomy or frenulectomy: Surgical procedure to eliminate the retraction or the movement of marginal gingiva or the interdental papilla by the action of the frenum by excising it. While frenotomy is the incision and the relocation of the frenal attachment. 1
Plack et al described a morphologic functional classification of labial frenum attachment as follows.
Aberrant or high frenum is a problem of inadequate attached gingiva, and mandibular frenum is of no clinical significance if an adequate zone of attached gingiva is present coronal to frenum but maxillary frenum may present asthenic problems or compromised orthodontic results. Two methods to check abnormal frenum attachment are as follows:
Tension test: Lip is moved outward, upwards for the upper, and downwards for the lower and also moved sidewards. If the marginal and oblique or interdental papilla moves away from the tooth surface, then the tension test is said to be positive
Blanch test: It is performed to diagnose a fleshy labial frenum. It is done by pulling the upper Lip outwards. Presence of thick and fleshy frenum is confirmed by the blanching of the incisive papilla region.
Procedures
Simple excision of frenum
Z-Plasty
Localized vestibulopasty with secondary epithelization is done when frenul attachment has a wide base
Frenectomy can be done by conventional scalpel technique or soft tissue lasers.2 There are various types of laser that are used in dentistry, including neodymium doped yttrium aluminium garnet (Nd:YAG), diode, carbon dioxide (CO2), erbium YAG (Er:YAG) and erbium, chromium:yttrium: scandium gallium-garnet (Er,Cr:YSGG) lasers.3 Each emits light at a specific wavelength that is determined by the gain medium (solid, liquid or gas).4 The Nd:YAG laser is a free-running pulsed laser that has a 1064-nm wavelength and is highly absorbed in melanin, less absorbed in haemoglobin, and slightly absorbed in water.5
Laser application in periodontics such as frenectomies, excision of gingival enlargement, gingivoplasties, gingival dipigmentation, operculum removal crown lengthening and biopsies of benign lesions are indicated for the laser treatment.6, 7, 8, 9
Advantage,of the laser during surgery are lesd pain, minimal bleeding, better visualization, minimal or no anesthesia, less damage to the adjacent tissues, and reduced risk of blood-born transmission of disease. And advantages after surgery are less scaring, faster healing of the operation, minimum post operative pain and reduced risk of post operative infection. 10
Aims & Objectives
The aim of the present study was to compare the degree of postoperative pain experienced by patients in frenectomy procedure with surgical scalpel and diode laser technique.
Materials and Methods
20 subject with an age range from 16-40 years old had participated in this study, there were all Systemically healthy, nonsmoker, good oral hygiene and who required labial frenulectomy were selected from the Out Patient Department of Periodontics, Buddha Institute of Dental Sciences & Hospital, Patna.
Informed written consent was obtained from the patients.
The patients were divided randomly into Group l and ll
Group l: Comprised of 10 patients selected for conventional scalpel technique
Group ll : Comprised of 10 patients selected for diode Laser technique.
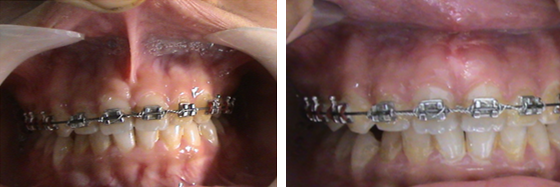
All the procedures were carried out by a single operator. For the conventional classical technique or scalpel technique proposed by Archer (1961) and as modified by Krugger (1964) was followed. The area was anesthetized with 2% lignocaine with 1:80,000 adrenaline. The frenum was held with a pair of hemostats, and the whole band of tissue together with its alveolar attachment was excised with a#15 blade. After freeing any remaining fibrous adhesions to the underlying periosteum, the wound was closed with 3’0 silk interrupted sutures. For the diode laser technique, the area was anesthetized with 2% lignocaine with 1:80,000 adrenaline. A diode laser 810 nm wavelength at power setting of 0.8 - 1.2 W made of fiber tip of diameter 300µ-400 µ was used in a contact mode and moved, in a paint brush stroke, from the base to the apex of the frenum there by excising it. Any remnant fibers over the periosteum were removed by gently sweeping the laser tip and the ablated remnant tissue was cleaned with gauze soaked in saline. Sutures were not given post the laser treatment. Both groups received postoperative instructions and the use of any analgesic was left to the patient's discretion.
Method of scoring
The patients were asked to rate the degree of pain during eating or speech, on a 10cm horizontal visual analog scale (VAS) by placing a vertical mark to assess position between the two endpoints. The left end point was nominated as "no pain," and the right end point was nominated as "unbearable pain." A single trained operator was engaged in recording the scores.
On the 7th day swelling, wound healing
Complete epithelization,
Incomplete epithelialization,
Ulcer,
Tissue defect or necrosis), and number of analgesics used were assessed. After 1st, 3rd and 7th day and after one month re evaluation of post operative pain was performed using same indices 11 for both the groups.
Results
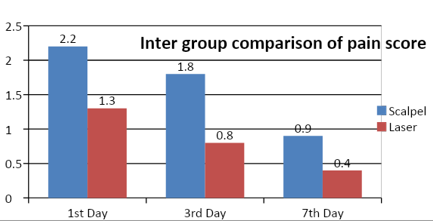
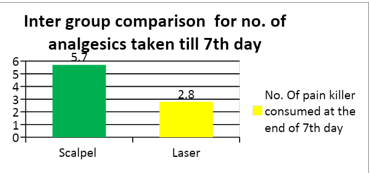
A total of 20 patients, (10 females and 10 males) completed the study. Comparison of the mean VAS score of the level of pain, for both groups, observed on the 1st, 3rd and 7th day of the study is summarized in (Figure 1, Figure 2, Figure 3). The analysis showed that VAS scores of pain on day 1, 3 and 7 were significantly lower in the laser group compared to the conventional technique. Number of analgesics used by Group l were significantly higher than Group ll.
Discussion
Periodontal plastic surgery is more conservative and precise technique that is practiced for the treatment of mucogingival problems. These are being practised to create more functional and aesthetic results. The presence of an aberrant frenum being one of the etiological factors for the persistence of a midline diastema and periodontal problems need greater attention. The aberrant frenum can be treated by frenectomy or by frenotomy procedures.6, 11 The soft tissue laser is now a viable alternative to the scalpel in soft tissue surgery. Lasers such as Nd:YAG, C02, and Er:YAG have been used for frenectomy procedures. Among these, CO, laser is the one most frequently used.6, 12 In the present study, diode laser, which characteristically uses a blend of gallium, arsenide, and other elements such as aluminum and indium, was used. The diode laser is now a viable alternative to the scalpel in soft tissue surgery. The wavelength of this laser is feebly absorbed in water, but extremely absorbed in hemoglobin and other pigments. Diode laser is considered as an excellent soft tissue laser as it doesn't interact with dental hard tissues and considering the affinity of the diode laser for wet tissue, it is readily applicable for most intraoral soft tissue surgery, including frenectomies.13, 14 In the present study, patients treated with the diode laser had significantly less postoperative pain both on day 1, day 3 and day 7 as compared to scalpel surgery as well as number of analgesics used were lower in the laser group. These findings are consistent with the other studies by Flaytac et al. 2 Butchibabu et al. 14 and Patel et al 15 wherein they suggested that soft tissue laser treatment used for frenectomy provides better patient perception in terms of postoperative pain and function than that obtained by the scalpel technique. The laser technique offers some advantages, such as a relatively bloodless surgical and post surgical event, the ability to precisely coagulate, vaporize, or cut tissue; sterilization of the wound site, minimal swelling and scarring, no suturing in most cases, little mechanical trauma, reduction of surgical time, decreased post surgical pain; and high patient acceptance. 16, 17 The increased pain perception associated with the scalpel frenectomy might be attributed to the fact that it is a more intrusive surgical procedure involving blood loss, wide surgical wound and suturing. The sutures also contribute to the discomfort postoperatively since they interfere with regular functions such as speech and intake of food. In addition, suture removal from gingival and labial tissues after 1 week can be painful because the sutures may be buried in the mucosa.11 To overcome these disadvantages, some clinicians use bio absorbable sutures after oral surgery.
Conclusion
In the present study diode laser frenectomy has presented with less post operative pain and discomfort and poor healing compared to conventional scalpel frenectomy. The increased pain in patients with scalpel technique could be attributed to the fact that it is a more intrusive procedure, wide surgical wound and suturing. The sutures could also contribute to discomfort.