- Visibility 92 Views
- Downloads 20 Downloads
- DOI 10.18231/j.ijpi.2019.031
-
CrossMark
- Citation
Endo perio lesions- A synergistic approach
- Author Details:
-
Shruthi Raveendran
-
Shruthi S
-
Parichaya Batra
-
Shirish A Magadum
-
Nisha K J *
Introduction
The three structures the tooth, the pulp and the periodontium supporting it forms a single biologic unit hence influencing each other during health, function and disease. This close inter relationship could result in concomitant lesions leading to the periodontal endodontic (perio endo) infections which has always been a challenge for the dental professionals to diagnose and manage. But it is of vital importance to make a correct diagnosis so that appropriate treatment plan can be provided.
The ectomesenchymal origin of both the pulp and periodontal tissues gives rise to anatomical connections, which remain throughout life.[1] The relationship between the periodontium and pulp was first discovered by Simring and Goldberg in 1964.[2]
In 2014, Al- Fouzan suggested a new endodontic periodontal interrelationship classification, based on the primary disease and its secondary effect.[3]
Retrograde periodontal disease
Primary periodontal lesion
Primary periodontal lesion with secondary endodontic involvement
Combined endodontic periodontal lesion
Iatrogenic periodontal lesion
This classification has increased the understanding of the origin and its disease process which is important for establishing the correct diagnosis and treatment with predictable success. The success rate of treating the endoperio lesions without a regenerative procedure ranges between 27- 37% which is very low.[4]
Inspite of the treatment of endo perio lesions being a multidisciplinary approach many times the periodontal aspect of the treatment plan is neglected due to various reasons making the endodontic therapy alone a failure. Hence in this case series we are aiming to discuss the endo perio cases treated with an endodontic treatment followed by a regenerative periodontal therapy /resective periodontal therapy with a follow up of up to 12 months.
Case Series
All the patients discussed below reported to the Department of Periodontics Vydehi Dental College and Hospital, Bangalore.
Case 1
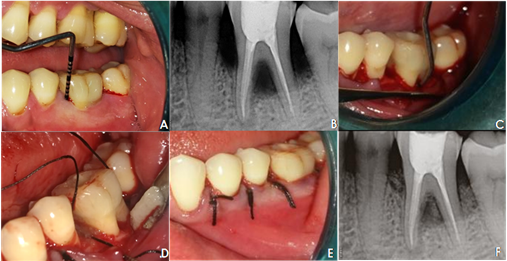
A male patient aged 45 years old reported with a chief complaint of pain in lower left back tooth region since a month. Clinical examination revealed the presence of periodontal probing depth of 6, 7, and 5 mm on mesiobuccal, mid buccal and disto buccal regions respectively and the presence of grade II furcation involvement in relation to 36. Tooth was non carious and showed negative response towards thermal and electric pulp test. Intra oral periapical radiograph showed the presence of an ill-defined radiolucency in the furcation area and an angular defect on the distal root surface extending up to middle third of the root. Hence the treatment plan included endodontic therapy first followed by periodontal regenerative therapy.
After successful endodontic treatment patient was posted for regenerative periodontal surgery. After administration of 2% local anaesthesia with 1:200000 adrenaline, using 15 no blade crevicular incision was given starting from distal line angle of 34 to mesial line angle of 37. Full thickness mucoperiosteal flap was reflected, defect was debrided and root planning was done using Hu-Friedy Gracey curettes, pre suturing was done followed by placement of Novabone putty in the defect region and flap was sutured using 3-0 silk suture followed by periodontal dressing and post-operative instructions were given. 12 months follow up of the patient showed complete resolution of the pain, reduction of probing pocket depth to 4mm and IOPAR showed significant bone fill in the furcation area and around the tooth.([Figure 1])
Case 2
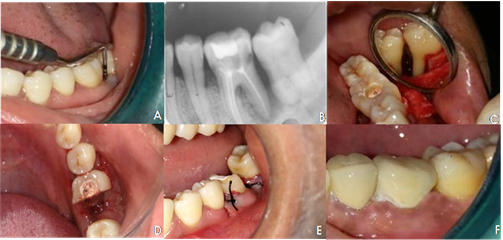
A 32-year-old female patient reported with a chief complaint of pain in lower left back tooth region since 6 months. On clinical examination 13mm probing depth was noted on distobuccal surface of 36 with grade I mobility. Tooth was non responsive to thermal and electric pulp testing. IOPAR showed complete radiolucency in distal root surface extending up to apical third of the root. Based on the clinical and radiographic investigations the treatment plan included an endodontic therapy followed by periodontal root resective therapy.
After the successful endodontic therapy, the patient was scheduled for root resective surgery. After administration of 2% local anaesthesia with 1:200000 adrenaline, crevicular incisions were made using a 15 no blade starting from mesial line angle of 35 to distal line angle of 37. Full thickness mucoperiosteal flap was reflected, defect was debrided and root planning was done using Hu-Friedy Gracey curettes. Distal portion of the tooth was resected using a carbide bur, and the resected portion was extracted. Flap was sutured using 3-0 silk suture followed by periodontal dressing.
6 months follow up showed uneventful healing and absence of mobility. Hence, prosthetic rehabilitation was done after 6 months ([Figure 2]).
Case 3
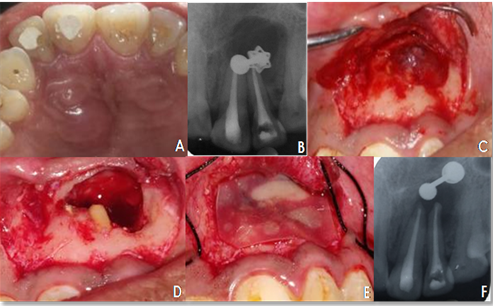
A 37 year old female patient reported with a chief complaint of pain and swelling in upper front tooth region since 15days. On clinical examination diffuse palatal swelling with normal probing depth and grade I mobility was present. It also revealed the presence of trauma from occlusion. Tooth showed negative response towards electric pulp testing. IOPAR showed well defined radiolucency in the periapical region of 21,22 suggestive of periapical cyst requiring an apicectomy procedure. Hence after the completion of endodontic therapy the patient was scheduled for apicectomy.
Endodontic therapy was done followed by which patient was taken up for apicoectomy. 2% local anaesthesia with 1:200000 adrenaline was administered, sub marginal incision was made using a 15 no blade, full thickness mucoperiosteal flap was reflected extending beyond the periapical region, using stainless steel bur window opening was done at the apex of the root and the cyst was exposed followed by enucleation of the cyst. The root end was resected followed by burnishing of the apical end. Presuturing was done. Platelet rich fibrin was placed in bony defect and guided tissue regeneration membrane (Healiguide) was used to cover the defect. Flap was sutured using 3-0 silk suture and periodontal dressing was given. Patient reported for suture removal after 10 days. Healing was satisfactory. 12 months revaluation of IOPAR showed a decrease in radiolucency in the periapical region and clinical revaluation showed the absence of tooth mobility. ([Figure 3])
Case 4
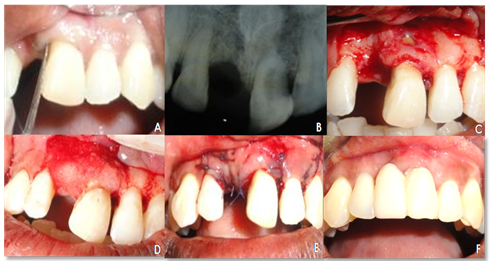
A 35year old female patient reported with a chief complaint of pain and pus exudation from upper front tooth region since a month. On clinical examination there was normal probing depth with pus exudation from gingival sulcus irt 21. Further examination revealed the presence of trauma from occlusion. 21 showed negative response to pulp vitality. Radiographic investigation showed a short root length. The prognosis was explained to the patient followed by all the treatment options. Since she insisted on retaining the tooth, we went ahead with endodontic therapy followed by periodontal regenerative therapy.
After initial phase I therapy, endodontic therapy was carried out followed by periodontal flap surgery under local anaesthesia. Crevicular incision were given and full thickness mucoperiosteal flap was reflected. Fenestration was noted at root apex and alveolar ridge defect in 11 region. Gutta percha was burnished at root apex and the fenestration area was closed using a GTR membrane. The alveolar defect was restored with Perioglas bone graft followed by placement of Periocol GTR. Flap was sutured and periodontal dressing was given.
Post-operative revaluation showed the presence of grade I mobility. To stabilize the tooth splinting was done and patient was put on maintenance therapy. Post 12months re-evaluation showed the resolution of clinical symptoms and reduction of mobility and the patient was given a permanent prosthesis ([Figure 4]).
Discussion
The successful treatment of end operio lesions always poses a major challenge. The key to success in treating these cases highly depends on thorough case history and clinical and necessary radiographic investigations to determine the cause and reach an exact diagnosis of the case. In addition, the ability of the clinician to categorize the lesion makes the treatment strategy clearer and more precise.
In the present case series several successful endodontic and periodontal cases were presented with different treatment modalities.
In all the reported cases we have first tried to achieve clean root canal system by which we have eliminated pain and which would help in gaining periapical seal. Different regenerative materials like Novabone putty, Platelet Rich fibrin, Perioglas and Perio Col GTR membrane were used.
The first two cases presented fell into the category of Primary periodontal lesion with secondary endodontic involvement. And the next two were the cases where the traumatic occlusion was the causative factor. Ideally the treatment plan in the last two cases should have included an orthodontic correction but as the patient was not willing to go for the orthodontic treatment and the prognosis for the same was questionable, we went ahead with an endodontic treatment followed by periodontal treatment.
In the first case we used Novabone putty as the regenerative material which has a bimodal particle distribution of calcium phosphosilicate with polyethylene glycol as an additive and glycerine as the binder. It has dual action of osteoconduction and osteostimulation.[5] It enhances the bone regeneration capacity by accelerating the resorption rate of the graft material. And in this case, it has successfully showed a regeneration in the furcation area and around the tooth.
In the second case as the distal root irt 36 was devoid of bone completely we could not go for a more conservative approach hence root resective periodontal therapy was the choice of treatment. Root resection can successfully treat specific furcation defects that cannot be solved by other surgical and non- surgical approaches.[6] Complications are not rare with these procedures but are usually unavoidable when specific endodontic, surgical and restorative guidelines are followed. In the present case patient was successfully treated and the missing half of the tooth was prosthetically restored after 6 months.
The third case presented radiographically with a huge periapical lesion suggestive of a perapical cyst which required apicectomy following endodontic treatment. It is a surgical procedure which consists of excision of pathological periapical tissue from the root surface along with surgical resection of the apical portion of the tooth, thus attaining regeneration and optimal healing. As lesion had eroded lot of bone, we attempted regenerating the same using PRF along with GTR membrane. PRF consists of an autologous leukocyte-platelet-rich fibrin matrix. [7],[8] Composed of a tetra molecular structure, with cytokines, platelets, and stem cells within it. [8],[9] Which acts as a biodegradable scaffold.[10] It acts as a reservoir of cells which is required for soft and hard tissue regeneration which has the capacity of sustained release of cells for 7 to 14 days by which it accelerates the healing process, hence aiming at faster healing with good regeneration.
The fourth case presented with a fenestration which was detected only after an intentional flap surgery was done. The fenestration in the present case could be due to the traumatic occlusion caused by her deep bite. The fenestration was restored with a GTR membrane. GTR membrane prevents the in growth of epithelium and fibroblast into the defect and thereby helps only the periodontal ligament cells to migrate and regenerate. GTR therapeutic protocol involves surgical placement of cell occlusive membrane facing the bone surface to physiologically seal off the site and create secluded space.[11]
The above all mentioned cases were treated with a multidisciplinary approach with expertise from endodontics and prosthodontics involved. In all the cases we were able to identify the repair and regeneration of the lost bone thereby increasing the longevity of teeth in turn improving its prognosis.
Conclusion
The ultimate goal of any dental treatment is the preservation and restoration of the function of natural tooth. And the treatment of any endo perio lesions always needs a multidisciplinary approach. Hence the synergistic approach towards a condition can definitely increase the longitivity of tooth.
Source of funding
None.
Conflict of interest
None.
References
- E Mandel, P Machton, M Torabinejad. Clinical diagnosis and treatment of endodontic and periodontal lesions. Quintessence Int 1993. [Google Scholar]
- M Simring, M Goldberg. The pulpal pocket approach: retrograde periodontitis. J Periodontol 1964. [Google Scholar]
- KS Al-Fouzan. New classication of endodontic periodontal lesions. Int J Dent 2014. [Google Scholar]
- JM Hirsch, Ahlstrom, P A Henrikson, G Heyden, L E Peterson. Periapical surgery. International Journal of Oral Surgery 1979. [Google Scholar]
- D N Umashankar, K S Kumar, R M Kumar, N Srinath, C Patil. Efficacy of calcium phosphosilicate as graft material in bony defects. Int J Oral Care Res 2018. [Google Scholar]
- M Desanctis, K G Murphy. The role of resective periodontal surgery in the treatment of furcation defects. Periodontology 2000. [Google Scholar]
- D M Dohan, J Choukroun, A Diss, S L Dohan, A J Dohan, J Mouhyi. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006. [Google Scholar]
- V Gupta, B K Bains, G P Singh, A Mathur, R Bains. Regenerative potential of platelet rich fibrin in dentistry: Literature review. Asian J Oral Health Allied Sci 2011. [Google Scholar]
- J Choukroun, A Diss, A Simonpieri, M O Girard, C Schoeffler, S L Dohan. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part IV: Clinical effects on tissue healing. . Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006. [Google Scholar]
- Q Li, S Pan, S J Dangaria, G Gopinathan, A Kolokythas, S Chu. Platelet-rich fibrin promotes periodontal regeneration and enhances alveolar bone augmentation. Biomed Res Int 2013. [Google Scholar]
- G Polimeni, K T Koo, M Qahash, A V Xiropaidis, J M Albandar, U M Wikesjo. Prognostic factors for alveolar regeneration: Effect of a space-providing biomaterial on guided tissue regeneration. J Clin Periodontol 2004. [Google Scholar]
How to Cite This Article
Vancouver
Raveendran S, S S, Batra P, Magadum SA, J NK. Endo perio lesions- A synergistic approach [Internet]. IP Int J Periodontol Implantol. 2019 [cited 2025 Sep 13];4(4):147-151. Available from: https://doi.org/10.18231/j.ijpi.2019.031
APA
Raveendran, S., S, S., Batra, P., Magadum, S. A., J, N. K. (2019). Endo perio lesions- A synergistic approach. IP Int J Periodontol Implantol, 4(4), 147-151. https://doi.org/10.18231/j.ijpi.2019.031
MLA
Raveendran, Shruthi, S, Shruthi, Batra, Parichaya, Magadum, Shirish A, J, Nisha K. "Endo perio lesions- A synergistic approach." IP Int J Periodontol Implantol, vol. 4, no. 4, 2019, pp. 147-151. https://doi.org/10.18231/j.ijpi.2019.031
Chicago
Raveendran, S., S, S., Batra, P., Magadum, S. A., J, N. K.. "Endo perio lesions- A synergistic approach." IP Int J Periodontol Implantol 4, no. 4 (2019): 147-151. https://doi.org/10.18231/j.ijpi.2019.031
