Introduction
Minimally Invasive Surgery (MIS) is a surgical technique that minimizes flap reflection and tissue trauma, resulting in stability of the blood clot within the wound site by maintenance of critical blood supply, tand hence reducing postoperative shrinkage over time. Microsurgery is the refined basic surgical technique that is made possible by the improvement in visual acuity with the use of surgical microscope. It has been broadly defined by Daniel RK. (1979)1 as surgical technique that is performed under magnification provided by operating microscope.
Periodontal microsurgery is defined as 'refinements in existing basic surgical techniques that are made possible by the use of surgical microscope and subsequent improved visual acuity' (Shanelec 1992). The treatment philosophy of micro surgery incorporates three principles:
History
Dentistry borrowed micro surgery from medicine since 1920s. From 1921-1960 microsurgery was utilized in different specialties and achieved better results than traditional surgery. In 1980 microsurgery was described by Serafin2 as a methodology - a modification and a refinement of recent surgical procedures. Surgeons have always endeavoured to treat surgical sites atraumatically. In 1921, Carl Nylen, who is considered the father of microsurgery, used a primitive binocular microscope for ear surgery. Most dental treatments historically had been rendered with unaided eyes. Magnification in microsurgical procedures were introduced in medicine during the late nineteenth century. In 1694, Anton van Leeuwenhook, an Amsterdam merchant constructed the first compound lens microscope. Periodontal microsurgery shares the attributes with medical microsurgery which will have a positive influence on its professional acceptance. Saemisch, a German ophthalmologist, introduced simple binocular loupes for an ophthalmic surgery in 1876. In 1950s, Barraquer JI3 began using the microscope in corneal surgeries. Apotheker and Jako first introduced the microscope to dentistry in 1978. In 1979 Daniel described micro surgery as “surgery performed under magnification”. Over the past decade, the field of periodontology has seen increased surgical refinement in many procedures. Periodontal microsurgery is the refinement of basic surgical techniques made possible by the improved visual acuity enabled by the use of surgical microscope. In the last decade, a special emphasis has been focused on the design and performance of surgical procedures for periodontal regeneration. Specific surgical approaches have been proposed to preserve the soft tissues and to reach a stable primary closure of the wound in order to seal the area of regeneration from the oral environment. The micro vessel surgery revolutionized plastic and transplantation surgery was mainly developed by neurosurgeons Jacobsen & Suarez 1960. In 1990, Wickham and Fitzpatric4 described the techniques of using smaller incisions as “minimally invasive surgery”. Hunter and Sackier in 1993 refines the concept of minimally invasive surgery, and described the surgical approach as “the ability to miniaturize our eyes and extend our hands to perform microscopic and macroscopic operations in places that could previously be reached only by large incisions”.
In 1996, Shanelec and Tibbetts showed a continuing-education course on periodontal microsurgery at the annual meeting of the American Academy of Periodontology which led to the development of centers devoted to teaching periodontal microsurgery. A long term prospective study by the same group reported on a two center study of 160 sites where MIS was used (Harrel, Wilson, & Nunn 2005).5 To lay more stress on wound and blood clot stability and primary wound closure for blood-clot protection, Cortellini and Tonetti6 proposed the Minimally Invasive Surgical Technique (MIST) in 2007. Belcher7 in 2001 summerized the benefits and potential usages of the surgical microscope in periodontal therapy. Cortellini and Tonetti8 later improvised it further by incorporating the concept of space provision for regeneration with the Modified Minimally Invasive Surgical Technique (M-MIST, Cortellini and Tonetti 2009).8 The use of operating microscopes, Surgical telescopes (loupes) and microsurgical instruments increased the surgical prognosis (Cortellini and Tonetti 2001, 2005).9,10 These instruments provided magnification and optimal illumination of the surgical field thereby improving the visual acuity. Trauma, orthognathic surgery, sialoendoscopy, and Temporo Mandibular Joint (TMJ) disorders in oral and maxillofacial surgery are usually performed with the support of the endoscopes. Application of endoscopic techniques in various surgeries has been approaching in deeper parts and still under experiment. Onishi11 in 1970, was the first to report arthroscopy of the human TMJ, and the first results were published by him (Onishi, 1975).
Principles
The proverb “you can do well what you see, if you see well what you do,” dates back to the 15th century when magnification was first used. The art of dentistry is based on precision. The human naked eye is capable of distinguishing fine details, but a better accomplishment can be made when an image is sharpened and enlarged. Microsurgery is an interesting concept in the minds of many dental professionals, and yet there are inabilities by most clinicians to perform such procedures which shows the dental profession’s lack of understanding of what microsurgery can truly accomplish. Periodontal microsurgery is a technique by which visual acuity is increased using a microscope at magnifications exceeding 10x. The introduction of loupes and surgical operating microscopes along with the micro-instruments has taken periodontal surgery to an altered level of sophistication and has made the microsurgical approach a stunning reality. Therefore this review highlights on application of Periodontal microsurgery in management of flap, root coverage procedures, periodontal regeneration and recently added implant surgical procedures.
It is the refinement of basic surgical technique that is achieved by improvement in visual acuity gained with the use of the surgical microscope.
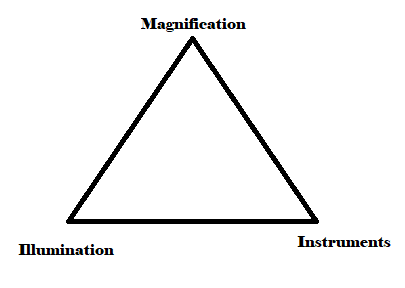
The three elements, i.e. magnification, illumination, and refined surgical skills by instruments are called the microsurgical triad (Belcher et al. 2001),7 the
improvement of which is a prerequisite for improved accuracy in surgical interventions. Without anyone of these, microsurgery is not possible.
Hand grips
The most commonly used precision grip in microsurgery is the pen grip or internal precision grip in which the thumb and index and middle fingers are used as a tripod. In a three-digit grip, an instrument to be used is held exactly as a pen would be held when writing. The forearm should be slightly supine, positioning the knuckles away so that the ulnar border of hand, wrist, and the elbow are all well supported, allowing the weight of the hand to be on the ulnar border. The middle finger should rest firmly and directly on either the working surface supporting the hand or indirectly on the ring finger and the middle finger holds the instrument. The thumb and index finger are so placed on the instrument so that it contacts the underlying middle finger. A very fine control can be obtained when the instrument is held with an internal precision grip and can be opened ad closed by will. If the middle finger is steady it will stabilize any tremor resulting from the thumb or index finger. The use of pen grip, relaxes the flexor and extensor muscles of the hand, that resists the fatigue, and as the intrinsic muscles that rotate the hand are well postured, the most accurate motion of which the hand is capable is obtained (e.g., rotational movement).
Magnification systems
There are a variety of simple and complex magnifying systems available, that includes three types of magnification loupes and the operating microscope. Both types of optical magnification have advantages and limitations. The mode of magnification used is often based on the task to be accomplished and the operator’s experience level. Whether or not more magnification is better must be weighed against the size of the viewing field and the depth of focus that occurs as magnification is increased. Increases in magnification require proportionate increases in field illumination.
Loupes
The most common magnification system used in dentistry is magnification loupes. Loupes are fundamentally two monocular microscopes, with side-by-side lenses, angled to focus on an object. The magnified image that is formed, has stereoscopic properties that are created by the use of convergent lens systems. Although loupes are widely used, their major disadvantage is that the eyes must converge to view an image, which can result in eye strain, fatigue and even vision changes with the prolonged use of poorly fitted loupes.
Loupe magnification
Wide ranges of magnifications are available in loupes, ranging from 1.5X to 10X. Loupes with less than 2X magnifications, are usually inadequate for the visual acuity necessary for microsurgery. For most periodontal procedures in which magnification is needed, loupes of 4X to 5X provide an effective combination of magnification, field size, and depth of focus.
Three types of loupes are commonly used:
Simple loupes
Simple loupes are composed of a pair of single, positive, side-by-side meniscus lenses. Each lens has two refracting surfaces, the first one occurs as light enters the lens and the other when it leaves. Simple loupes offer magnification upto 1.5 x only. Its main advantage is that it is cost effective. But they are primitive with limited capabilities, they are highly subjected to spherical and chromatic aberration, which distorts the image of the object they have no practical dental application beyond a magnification range of 1.5 diameters, Because of their size and weight limitations. And they sacrifice depth of field for working distance, when positioned close to the eye, when positioned close to the object viewed, they sacrifice working distance for depth of field.
Compound loupes
Compound loupes possess converging multiple lenses with intervening air spaces that gain additional refracting power, magnification, working distance, and depth of field. They can be adjusted to clinical needs without excessive increase in size or weight. They can be achromatic that have an improved optical design and contain of two glass pieces, usually bonded together with clear resin.
Prism loupes
They are the most optically advanced type of loupe magnification presently available. They lengthen the light path by virtually folding the light so that the barrel of the loupe can be shortened. They are superior to other loupes in terms of better magnification, wider depths of field, longer working distances and larger fields of view. The barrels of prism loupes are short and can be mounted on eyeglasses or a headband. But the increased weight, at magnifications of 3.0 diameters or greater, causes headband mounted loupes to be more comfortable and stable than mountings on glasses.
Operating microscope
The properly equipped operating microscope is vastly superior to magnifying loupes as they are flexible and comfortable in optical magnification. The operating microscope can be simple to use with proper instructions and a good practice. It is, however, much more expensive and initially more difficult to use. Operating microscopes combine the magnification of loupes with a magnification changer and a binocular viewing system. The parallel binoculars protect against eyestrain and fatigue. Operating microscopes incorporate fully coated optics and achromatic lenses with high-resolution and high-contrast stereoscopic vision. Operating microscopes are designed on Galilean principles.
Proper instrumentation is fundamental for microsurgical intervention. A basic set comprises of a needle holder, micro scissors, micro scalpel holder, anatomic and surgical forceps, and a set of various elevators. A varied type of ophthalmic knives like the crescent, lamellar, blade breaker, sclera and spoon knife can be used in the field of Periodontics. They offer the dual advantages of extreme sharpness and smaller size. This helps limit tissue trauma and promotes faster healing. As these knives are chemically etched rather than ground, and their sharper blades produce a more precise wound edge.
In order to guarantee atraumatic surgical approach in the MIPS, the use of miniaturized operation instruments is considered to be of great importance (Gassmann G et al, 2006).12
Generally, a useful microsurgical tray for the routine use in MIPS should include:
Knives and scalpel blades
The knives which are commonly used in periodontal microsurgery are those which are used in ophthalmic surgery or plastic surgery. Different type of knifes are used. The crescent knife are used for intra-sulcular procedures. The spoon knives are often used to undermine the lateral sulcular region to prepare placement of connective tissue grafts using a sulcular, non-relief technique. Blades include minicresent microsurgical blade. Microsurgical incisions are established at a 90-degree angle to the surface using microsurgical scalpels.
Microscissors
These are used for cutting the tissues, blood vessels, and nerves. The commonly used microscissors are 14 cm and 18 cm long. A 9 cm microscissors are preferable to handle delicate tissues. Straight scissors cut sutures and trim the adventitia of vessels or nerve endings. Curved scissors cut vessels and nerves.
Microforceps
These are used to handle small delicate tissues without damaging them and to hold fine sutures while tying knots. Jeweler forceps are strong and can even be used to separate minute vessels and nerves.
Micro needle holder
It is used to grasp the needle, pull it through the tissues, and tie knots. The needle is to be held between its middle and lower thirds at its distal tip. If held too close to the top, the anastomosis between the two ends of the vessel cannot be completed with a single stitch. Maintaining steady control is difficult, if held too close to the bottom and the direction of the tip can be changed easily. A titanium needle holder is the best choice.
Needles
In order to minimize tissue trauma in microsurgery, the sharpest needles, reverse cutting needles with precision tips or spatula needle with micro tips are preferred. A 3/8” circular needle generally ensures good results for various periodontal surgical procedures.
Suture material
Although 4-0 or 5-0 sutures are typically used in Periodontics, in periodontal microsurgery 6-0 and 7-0 sutures are used.
Sutures
One of the three basic rules of microsurgery is attention to passive wound closure. The desired result is achieved by exact primary closure of the wound edge. Ideally, the incisions should be almost invisible and closed with precisely placed, small sutures with minimal tissue damage and very minimal bleeding. With all of the surgical subspecialties, suture materials and techniques have evolved to the point that sutures are designed and developed for specific procedures. What has been developed for medicine is subsequently used in dentistry. A small to very small needles of a finegauge material are used for microsurgery. They are designed for maximum needle holder stability. It has a significant impact on the entire suturing procedure. The surgeon must have the utmost control of the needle in the holder when passing through the tissue. So, the needle holder must be appropriately sized for the needle and suture that is being selected.
Suture Geometry
The microsurgery depends on careful, non invasive entry incisions and dissection to allow passive wound closure. This is followed by wound closure using the fundamental geometric approach, with the goal of primary and passive wound closure. The geometry of microsurgical suturing consists of the following points (Price PB, 1948).13
Wound healing in microsurgery
Microsurgery encourages repair through primary healing, which is rapid and requires less formation of granulation or scar tissue. Studies show closure of microsurgical wounds within 48 hours. Secondary wound healing is slower because new tissue formation is required to fill voids at the edge of the partially closed wound. since surgical trauma is less during microsurgery, there is less cell damage and necrosis, that leads to less inflammation and pain.
Microsurgical Indications In Periodontal Surgery
Incisions
The incisions for Minimally Invasive Periodontal Surgery (MIPS) are designed to conserve as much of the soft tissue as possible. Using Tunnel Technique (TT) in periodontal surgery is an important criteria of MIPS. This technique is originated primarily from the Envelope Technique (ET) developed by Raetzke14 in 1985 for the treatment of single gingival recessions. In the TT, intrasulcular incisions are first initiated and then followed by supraperiosteal preparation of a tunnel through the defect areas. This will allow the transplantation of Sub-Epithelial Connective Tissue Graft (SECTG) in the sulcular areas.
In terms of MIPS, and talking about SECTG, it is important to mention that the Single Incision Technique (SIT), for the extraction of SECTG from the palate, is more preferable than using Trap Door Incision Technique (TDIT).
Flap elevation
In MIPS, the tissue is elevated utilizing sharp dissection using Orban’s knives that are one third their original size. The use of the small Orban knives will allow the blade to be placed into the previously made intrasulcular incision and, with the tip angled toward the center of the papilla, perform a thinning and undermining incision.
It is always recommended to achieve the incisions for flap elevation in the form of “splitting,” so that the periosteum tissue is left on the bone surface. By leaving the periosteum in its original position, a coronally tension free reflection of the flap will be more possible, and moreover, less postsurgical bone loss and edema are to be expected (Gassmann G et al in 2006).12
Modified papilla preservation technique: Cortellini et al. modified the Papilla preservation technique described by Takei et al in 1985. This technique was introduced as a new approach for interproximal regenerative procedures called ‘the modified papilla preservation technique’. This technique is performed in wide interdental spaces (2 mm). The main advantage of this technique includes primary closure of tissues and papilla preservation in 75% of cases.
A horizontal incision is performed on the buccal papillary tissue at the base of the papilla. A full-thickness palatal flap, which includes the interdental papilla, is elevated. A buccal full-thickness flap is elevated with vertical releasing incisions and/or periosteal incisions, when needed. The interdental tissues are repositioned and sutured to completely cover the membrane. A horizontal internal crossed mattress suture is placed below the mucoperiosteal flap between the base of the palatal papilla and the buccal flap. This suture relieves all the tension of the flaps. A second suture (vertical internal mattress suture) is placed between the buccal aspect of the interproximal papilla and the most coronal portion of the buccal flap to ensure primary closure. This technique is performed in wide interdental spaces (2 mm), especially in the anterior region. This technique allows for achieving primary closure of the tissue and preserving the papilla in 75% of cases.
Simplified papilla preservation flap
The SPPF is applicable in narrow interdental spaces (< 2 mm). An oblique incision across the defect-associated papilla, from the gingival margin at the buccal line angle of the involved tooth to the mid-interproximal portion of the papilla under the contact point of the adjacent tooth is given. A full-thickness palatal flap including the buccal papilla is elevated. Cortellini15 et al in 1999 proposed the Simplified Papilla Preservation Flap (SPPF).
It is initiated with an oblique incision across the defect-associated papilla, from the gingival margin at the buccal line angle of the involved tooth to the mid-interproximal portion of the papilla below the contact point of the next tooth. A full-thickness flap from the palatal aspect, with the papilla, and a split-thickness flap from the buccal aspect are then elevated. The interdental tissues are positioned and sutured to obtain primary closure of the interdental space. The SPPF is performed in narrow interdental spaces (2 mm).
Both these techniques are important elements in terms of MIPS since they can guarantee minimal access to the periodontal defect.
In mucogingival surgery
All the techniques tend to have various degrees of therapeutic results since they are technique and operator sensitive. A more consistent way of achieving mucogingival surgical treatment results is by the use microsurgical methods and practice, which itself has a long learning curve to obtain desired treatment outcomes.
Microsurgery in periodontics has proven to be an effective way of improving the predictability of gingival transplantation procedures used in treating recession along with reduced operative trauma and discomfort. Correct diagnosis, with microsurgical techniques, makes complete root coverage extremely predictable in class I and class II marginal tissue recession defects with a variety of procedures. The partial root coverage results achieved in class III and class IV marginal recession with conventional surgery can also be greatly enhanced through the use of microsurgery.
Root Coverage Procedures
Success of root coverage procedure involves dexterity of surgeon an excellent visualization of the operating field, and of course an atraumatic surgical approach, . All these factors can be fulfilled using a surgical microscope. It has to be realized that factors influencing the degree of coverage such as root preparation, delicate tissue handling, tissue thickness and meticulous plaque control have to be controlled in order to maximize treatment outcomes.
Papilla Reconstruction Procedures
The reconstruction of lost interdental papillae remains a challenge. Among all techniques microsurgical procedure is an atraumatic procedure to position donor tissue under a deficient interdental papilla. Because of the small dimensions of the interdental papilla and the limited access, surgical magnification and microsurgical instruments are useful.
Restoring the Edentulous Ridge
There are a variety of techniques using microsurgical approach. In addition to establishing adequate vertical height, sufficient soft tissue thickness must be created to provide an emergence profile for pontics or a dental implant prosthesis.
Microsurgeries & implants
Dental implantology has evolved over the years, but patient acceptance is still not wide, because of the expenses and durations which are required to attain a functional status. Over the past three decades literature has documented the high long term success of dental implants which utilizing conventional Brånemark two stage protocol, which allows a load free healing period of three to six months. The actual need of healing periods of such durations has been greatly questioned, because they were determined on an empirical basis (De Vasconsellos DK,et al in 2006).16
The one-piece system of implants allows for better tissue healing by better adhesion of the gingival mucosa to form a collar which is healthy and adherent to the implant, and avoiding a second surgical procedure (Prithviraj DR, et al 2013).17 The prosthetic procedure of a one-piece implant enables the physiological structure of the tooth surrounding tissues by enabling a borderline preparation that follows the contour of the gingival margin leading to a better preservation of mucousal seal (Barrachina-Díez JM et al in 2013).18
One piece immediate loading implants have a survival rate similar to delayed loading implants (Shigehara S, et al in 2014).19 Immediate loading of one-piece implants has become a widely used procedure since it is a boon to partially edentulous patients.
Sinus floor elevation
Modifications of the conventional techniques have been suggested by various authors and thus the ‘Minimally invasive Techniques’ have come to stay (Efraim Kfir et al in 2013).20 Finding an alternative method for sinus augmentation led to the evolution of the “The innovative implant technology (IIT) Sinu Lift System” one of the minimally invasive indirect sinus lift instrument. This technique becomes more predictable if used in combination with PRP and β –TCP mix which may result in an increased rate of bone formation and sinus augmentation. It is appropriate to state that sinus-floor elevation using the “sinu-lift system” is definitely a reliable tool in achieving maximum sinus lift for augmentation. Future directions should see a more pivotal role to be played by this method of sinus lift prior to implant placement and it has obvious advantages, paving the way for maximal augmentation for successful implant placement, while using minimally invasive techniques. The proposed technique is minimally invasive, decreases the chair time, makes implant dentistry more accurate with predictable out comes and increases the comfort level for implant patients.
Lasers in minimally invasive periodontal Therapy
‘Pain free’ and ‘simple procedure’ are two of the most attractive phrases to patients who are otherwise reluctant to accept any dental treatment (van Wijk AJ et al in 2008).21 Minimally invasive dental therapy (Jingarwar MM et al 2014)22 could satisfy the demands of such patients. The procedures can be comfortable, although not necessarily without any pain; and be effective for disease control whilst preserving more healthy dental tissue.
The delivery of laser power through a fine laser tip enables the practitioner to perform precise and small procedures with minimal damage around the treated site. Such a precise treatment modality is essential for performing minimally invasive periodontal treatments.
Discussion
Minimally invasive procedures are the new paradigm in health care. Major critical surgeries from heart bypasses to gall bladder, surgeries are being performed with these techniques. Dentistry is joining this exciting revolution as well. Minimally Invasive Dentistry (MID) was defined as a concept that preserves dentition and supporting structures. Minimally invasive dentistry adopts a philosophy that integrates prevention, remineralisation and minimal intervention for the placement and replacement of restorations. With the advances in dental technology, the access and visualization of these surgical sites were possible, despite their smaller incisions and openings. The term “minimally invasive surgery” (MIS) was first coined by the general surgeons Fitzpatrick and Wickham 4 in 1990. They defined minimally invasive surgery as the ability to perform a traditional surgical procedure and achieve the same or better outcomes utilizing a surgical opening that was smaller than the traditional surgical access. These procedures were initially described by the instrument used to perform it, for example, laparoscopic surgery or microsurgery.
Summary and Conclusion
The goal of periodontal surgery has always been to alleviate or eliminate the degeneration associated with progressive periodontal disease and to regenerate lost tissues. Introduction of minimally invasive surgery highlights various advantages such as less invasive surgery, shorter duration, favoured healing due to improved wound stability of minimally mobilized flaps, and benefitting the patient with reduced intra operative and postoperative morbidity. Magnification systems have opened up a whole new world for the surgeon in many specialties. In implants, a single stage, one piece implant placement with immediate loading provides a good soft tissue healing and minimal post operative discomfort to the patient. Flapless surgery, reported a high success rate with minimal post operative swelling or pain experiences and a minimal need for analgesics. Thus, single stage one piece implant placement, immediate loading, and a trans-mucosal flapless surgery is minimally invasive and provide greater advantages, with high acceptance by the surgeons as well as the patients.
New laser generations offer a precise control in tissue cutting, for different procedures and corresponding to diverse tissue biotypes, cutting cleanly the soft tissues, with good haemostasis and high comfort for the patient. One of the big advantages of dental laser medicine is the possibility to do more, with less anaesthetic and smaller injury of the dental tissue. These advantages convert laser therapy into a necessary element for the future dental practice, and also in the other medical fields. It is essential for the dentists to be informed and trained on the lasers’ technical features and, also, on the multiple applications of lasers in dentistry. The future promises further evolution towards a more primary preventive lesser invasive approach, facilitated by emerging technologies for diagnosis, prevention and treatment. However, there are technical, cultural and economic obstacles to overcome for this to be fully realized in clinical practice.